Pregnancy SmartSiteTM
Breast cancer - self-care for lymphedema; Mastectomy - self-care for lymphedema DescriptionLymphedema is the buildup of lymph in your body. Lymph is a fluid surrounding tissues. Lymph moves through vessels in the lymph system and into the bloodstream. The lymph system is a major part of the immune system. What is LymphedemaWhen lymph builds up, it can cause an arm, leg, or another area of your body to swell and become painful. The disorder can be lifelong. What to ExpectLymphedema may start 6 to 8 weeks after surgery or after radiation treatment for cancer. It can also start very slowly after your cancer treatment is over. You may not notice symptoms until 18 to 24 months after treatment. Sometimes it can take years to develop. Ways to Help Relieve SwellingUse your arm that has lymphedema for everyday activities, such as combing your hair, bathing, dressing, and eating. Rest this arm above the level of your heart 2 or 3 times a day while you are lying down.
Taking Care of Your SkinEvery day, clean the skin of your arm or leg that has lymphedema. Use lotion to keep your skin moist. Check your skin every day for any changes. Protect your skin from injuries, even small ones:
Take care of your feet:
Don't put too much pressure on your arm or leg with lymphedema:
Taking care of cuts and scratches:
Taking care of burns:
Living with lymphedema can be hard. Ask your provider about visiting a physical therapist who can teach you about:
If you are prescribed a compression sleeve:
When to Call the DoctorContact your provider if you have any of these symptoms:
ReferencesDoroshow JH. Approach to the patient with cancer. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 164. National Cancer Institute website. Lymphedema (PDQ) - health professional version. www.cancer.gov/about-cancer/treatment/side-effects/lymphedema/lymphedema-hp-pdq. Updated April 30, 2024. Accessed May 29, 2024. Spinelli BA. Clinical conditions in patients with breast cancer. In: Skirven TM, Osterman AL, Fedorczyk JM, eds. Rehabilitation of the Hand and Upper Extremity. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 115. | |
| |
Review Date: 3/31/2024 Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

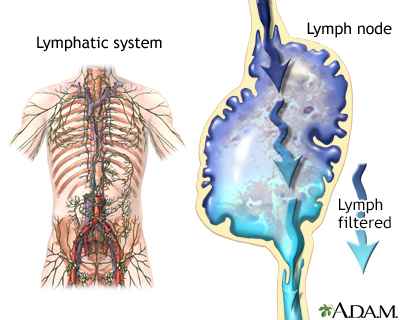 Lymphatic system
Lymphatic system
