Pregnancy SmartSiteTM
Partial lung collapse DefinitionAtelectasis is the collapse of part or, much less commonly, all of a lung. CausesAtelectasis is caused by a blockage of the air passages (bronchus or bronchioles) or by pressure on the outside of the lung. Atelectasis is not the same as another type of collapsed lung called pneumothorax, which occurs when air escapes from the lung. The air then fills the space outside of the lung, between the lung and chest wall. In atelectasis, there is usually fluid between the lung and the chest wall and the air sacs within the lung fill with fluid. Common situations in people with atelectasis include:
Atelectasis is common after surgery or in people who are or were in the hospital. Risk factors for developing atelectasis include:
SymptomsSymptoms may include any of the following: There are no symptoms if atelectasis is mild. Exams and TestsTo confirm if you have atelectasis and determine its cause, the following tests will likely be done to view the lungs and airways:
TreatmentThe goal of treatment is to treat the underlying cause and re-expand the collapsed lung tissue. If fluid is putting pressure on the lung, removing the fluid may allow the lung to expand. Treatments include one or more of the following:
Outlook (Prognosis)In an adult, atelectasis in a small area of the lung is usually not life threatening. The rest of the lung can make up for the collapsed area, bringing in enough oxygen for the body to function. Large areas of atelectasis may be life threatening, often in a baby or small child, or in someone who has another lung disease or illness. The collapsed lung usually reinflates slowly if the airway blockage has been removed. Scarring or damage may remain. The outlook depends on the underlying disease. For example, people with extensive cancer often don't do well, while those with simple atelectasis after surgery have a very good outcome. Possible ComplicationsPneumonia may develop quickly after atelectasis in the affected part of the lung. When to Contact a Medical ProfessionalContact your health care provider right away if you develop symptoms of atelectasis. PreventionTo prevent atelectasis:
ReferencesFrohlich M, Prentice B, Jaffé A. Air and fluid in the pleural space, and atelectasis. In: Bush A, Deterding R, Li AM, et al. Kendig and Wilmott's Disorders of the Respiratory Tract in Children. 10th ed. Philadelphia, PA: Elsevier; 2024:chap 81. O'Donnell AE. Bronchiectasis, atelectasis, and cavitary or cystic lung diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 78. Rozenfeld RA. Atelectasis. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 459. | |
| |
Review Date: 8/19/2024 Reviewed By: Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutgers New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

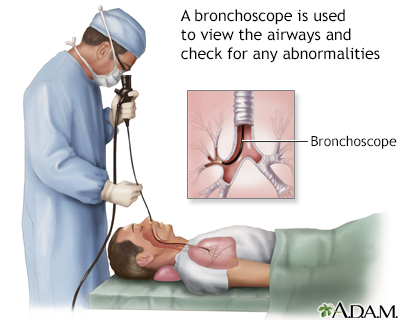 Bronchoscopy
Bronchoscopy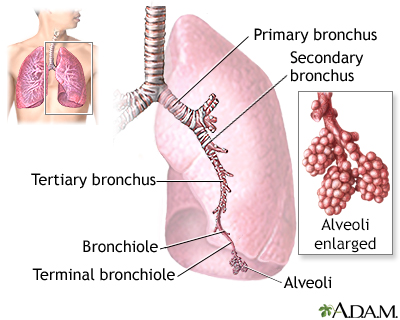 Lungs
Lungs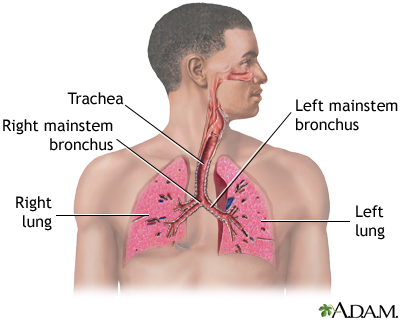 Respiratory system
Respiratory system
