Pregnancy SmartSiteTM
DVT; Blood clot in the legs; Thromboembolism; Post-phlebitic syndrome; Post-thrombotic syndrome; Venous - DVT DefinitionDeep vein thrombosis (DVT) is a condition that occurs when a blood clot forms in a vein deep inside a part of the body. DVT mainly affects the large veins in the lower leg and thigh, but can occur in other deep veins, such as in the arms and pelvis. DVT most often affects only one side of the body. CausesDVT is most common in adults over age 60. But it can occur at any age. When a clot breaks off and moves through the bloodstream, it is called an embolism. An embolism can get stuck in the blood vessels in the brain, lungs, heart, or another area, leading to severe damage. Blood clots may form when something slows or changes the flow of blood in the veins. Risk factors include:
Blood is more likely to clot in someone who has certain problems or disorders, such as:
Sitting for long periods when traveling can increase the risk for DVT. This is most likely when you also have one or more of the risk factors listed above. SymptomsDVT mainly affects the large veins in the lower leg and thigh, most often on one side of the body. The clot can block blood flow and cause:
Exams and TestsYour health care provider will perform a physical exam. The exam may show a red, swollen, or tender leg. Tests that are often done to diagnose a DVT are:
Blood tests may be done to check if you have an increased chance of blood clotting, including:
TreatmentYour provider will give you medicine to thin your blood (called an anticoagulant). This will keep more clots from forming or old ones from getting bigger. Heparin is often the first medicine you will receive.
One type of blood-thinning medicine called warfarin (Coumadin or Jantoven) may be started along with heparin. Warfarin is taken by mouth. It takes several days to fully work. Another class of blood thinners are called direct oral anticoagulants (DOAC), including:
These medicines work in a similar way to heparin and can be used right away in place of heparin. Your provider will decide which medicine is right for you. You will most likely take a blood thinner for at least 3 months. Some people take it longer, or even for the rest of their lives, depending on their risk for another clot and for bleeding. When you are taking a blood thinning medicine, you are more likely to bleed, even from activities you have always done. If you are taking a blood thinner at home:
In rare cases, you may need a procedure instead of or in addition to anticoagulants. These may involve:
Follow any other instructions you are given to treat your DVT. Outlook (Prognosis)DVT often goes away without a problem, but the condition can return. The symptoms can appear right away or you may not develop them for one or more years afterward. Wearing compression stockings during and after the DVT may help prevent this problem. Possible ComplicationsComplications of DVT may include:
When to Contact a Medical ProfessionalContact your provider if you have symptoms of DVT. Go to the emergency room or call the local emergency number (such as 911) if you have DVT and you develop:
PreventionTo prevent DVT:
ReferencesAziz MU, Zahid M, Weber TM, Robbin ML. Peripheral veins. In: Rumack CM, Levine D, eds. Diagnostic Ultrasound. 6th ed. Philadelphia, PA: Elsevier; 2024:chap 26. Chan NC, Weitz JI. Venous thromboembolism. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 140. Kabrhel C. Pulmonary embolism and deep vein thrombosis. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 74. Stevens SM, Woller SC, Kreuziger LB, et al. Antithrombotic therapy for VTE disease: second update of the CHEST guideline and expert panel report. Chest. 2021;160(6):e545-e608. PMID: 34352278 pubmed.ncbi.nlm.nih.gov/34352278/. Weitz JI, Eikelboom JW. Venous thrombosis and embolism. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 68. | |
| |
Review Date: 4/1/2025 Reviewed By: Linda J. Vorvick, MD, Clinical Professor Emeritus, Department of Family Medicine, UW Medicine, School of Medicine, University of Washington, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Deep venous thromb...
Deep venous thromb...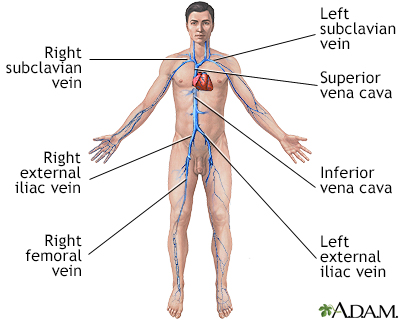 Deep veins
Deep veins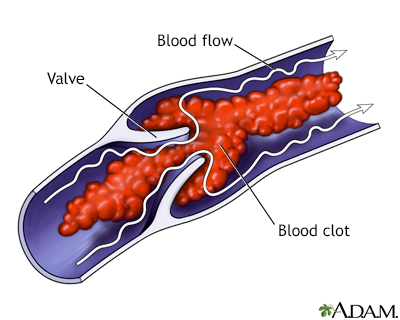 Venous blood clot
Venous blood clot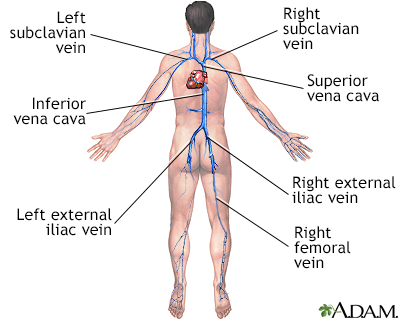 Deep veins
Deep veins
