Pregnancy SmartSiteTM
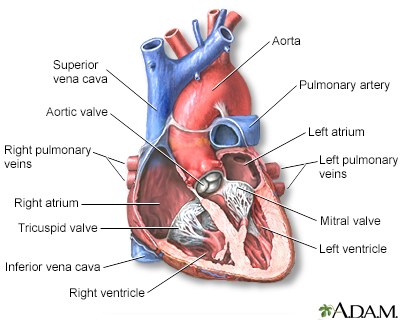
Mitral valve regurgitation; Mitral valve insufficiency; Heart mitral regurgitation; Valvular mitral regurgitation DefinitionMitral regurgitation is a disorder in which the mitral valve on the left side of the heart does not close properly. Regurgitation means leaking from a valve that does not close all the way. CausesBlood that flows between different chambers of your heart must flow through a valve. The valve between the 2 chambers on the left side of your heart is called the mitral valve. It opens up enough so that blood can flow from the upper chamber of your heart (left atrium) to the lower chamber (left ventricle). It then closes, keeping blood from flowing backwards.  When the mitral valve doesn't close all the way, blood flows backward into the upper heart chamber (atrium) from the lower chamber as it contracts. This is called mitral regurgitation and is a common type of heart valve disorder. This cuts down on the amount of blood that flows to the rest of the body. As a result, the heart may try to pump harder. This may lead to congestive heart failure. Mitral regurgitation may begin suddenly. This often occurs after a heart attack. When the regurgitation does not go away, it becomes long-term (chronic). Many other diseases or problems can weaken or damage the valve or the heart tissue around the valve. You are at risk for mitral valve regurgitation if you have:
Another important risk factor for mitral regurgitation is past use of a diet pill called "Fen-Phen" (fenfluramine and phentermine) or dexfenfluramine. The drug was removed from the market by the U.S. Food and Drug Administration (FDA) in 1997 because of safety concerns. SymptomsSymptoms may begin suddenly if:
There are often no symptoms. When symptoms occur, they often develop gradually, and may include:
Exams and TestsWhen listening to your heart and lungs, the health care provider may detect:
The physical exam may also reveal:
The following tests may be done to look at the heart valve structure and function:
Cardiac catheterization may be done if heart function becomes worse. TreatmentTreatment will depend on what symptoms you have, what condition caused the mitral valve regurgitation, how well the heart is working, and if the heart has become enlarged. People with high blood pressure or a weakened heart muscle may be given medicines to reduce the strain on the heart and ease symptoms. The following medicines may be prescribed when mitral regurgitation symptoms get worse:
A low-sodium diet may be helpful. You may need to limit your activity if symptoms develop. Once the diagnosis is made, you should visit your provider regularly to track your symptoms and heart function. You may need surgery to repair or replace the valve if:
Catheter based non-surgical techniques to place clips or replace the mitral valve are increasingly in use for some selected patients with mitral regurgitation. Outlook (Prognosis)The outcome varies. Most of the time the condition is mild, so no therapy or restriction is needed. Symptoms can most often be controlled with medicine. Possible ComplicationsProblems that may develop include:
When to Contact a Medical ProfessionalContact your provider if symptoms get worse or do not improve with treatment. Also contact your provider if you are being treated for this condition and develop signs of infection, which include:
PreventionPeople with abnormal or damaged heart valves are at risk for an infection called endocarditis. Anything that causes bacteria to get into your bloodstream can lead to this infection. Steps to avoid this problem include:
ReferencesCarabello BA, Kodali S. Valvular heart disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 60. Hahn RT, Bonow RO. Mitral regurgitation. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 76. Writing Committee Members, Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Thorac Cardiovasc Surg. 2021;162(2):e183-e353. PMID: 33972115 pubmed.ncbi.nlm.nih.gov/33972115/. | |
| |
Review Date: 2/27/2024 Reviewed By: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Heart - section th...
Heart - section th...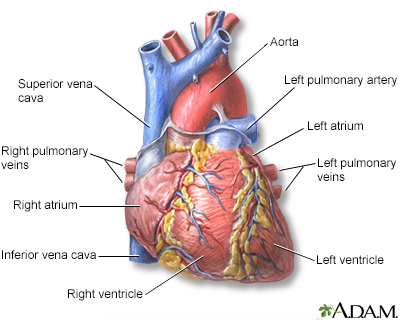 Heart - front view
Heart - front view
