Pregnancy SmartSiteTM
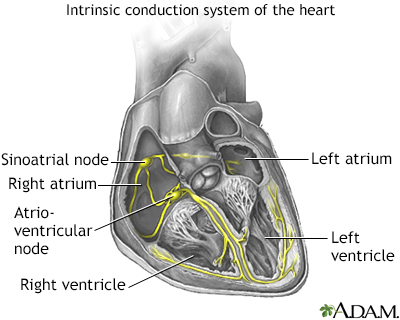
PSVT; Supraventricular tachycardia; Abnormal heart rhythm - PSVT; Arrhythmia - PSVT; Rapid heart rate - PSVT; Fast heart rate - PSVT DefinitionParoxysmal supraventricular tachycardia (PSVT) is episodes of a rapid heart rate that start in a part of the heart above the ventricles. "Paroxysmal" means from time to time. CausesNormally, the chambers of the heart (atria and ventricles) contract in a coordinated manner.
 The rapid heart rate from PSVT may start with events that occur in areas of the heart above the lower chambers (ventricles). There are a number of specific causes of PSVT. It can develop when doses of the heart medicine, digitalis, are too high. It can also occur with a condition known as Wolff-Parkinson-White syndrome, which often causes symptoms in young people and infants. The following increase your risk for PSVT:
SymptomsSymptoms most often start and stop suddenly. They can last for a few minutes or several hours. Symptoms may include:
Other symptoms that can occur with this condition include: Exams and TestsA physical exam during a PSVT episode will show a rapid heart rate. It may also show forceful pulses in the neck. The heart rate may be over 100, and even more than 250 beats per minute (bpm). In children, the heart rate tends to be very high. There may be signs of poor blood circulation such as lightheadedness. Between episodes of PSVT, the heart rate is normal (60 to 100 bpm). An electrocardiogram (ECG) during symptoms shows PSVT. An electrophysiology study (EPS) may be needed for an accurate diagnosis and to find the best treatment. Because PSVT comes and goes, to diagnose it people may need to wear a 24-hour Holter monitor. For longer periods of time, another type of the rhythm recording device may be used. 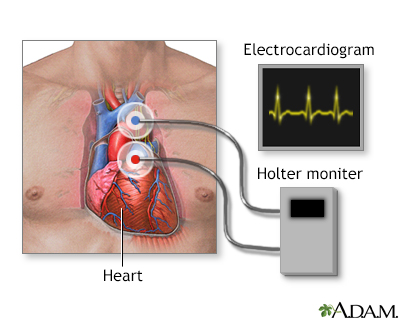 TreatmentPSVT that occurs only once in a while may not need treatment if you don't have symptoms or other heart problems. You can try the following techniques to interrupt a fast heartbeat during an episode of PSVT:
You should avoid smoking, caffeine, alcohol, and illicit drugs. Emergency treatment to slow the heartbeat back to normal may include:
Long-term treatment for people who have repeat episodes of PSVT, or who also have heart disease, may include:
Outlook (Prognosis)PSVT is generally not life threatening. If other heart disorders are present, it can lead to congestive heart failure or angina. When to Contact a Medical ProfessionalContact your health care provider if:
It is especially important to contact your provider if you also have other heart problems. ReferencesDalal AS, Van Hare GF. Disturbances of rate and rhythm of the heart. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 462. Kalman JM, Sanders P. Supraventricular tachycardias. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 65. Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/ HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2016;133(14);e471-e505. PMID: 26399662 pubmed.ncbi.nlm.nih.gov/26399662/. Zimetbaum P, Goldman L. Supraventricular ectopy and tachyarrhythmias. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 52. | |
| |
Review Date: 2/27/2024 Reviewed By: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

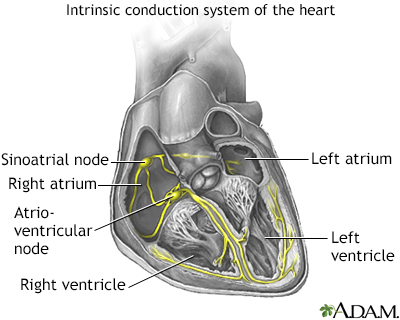 Conduction system ...
Conduction system ...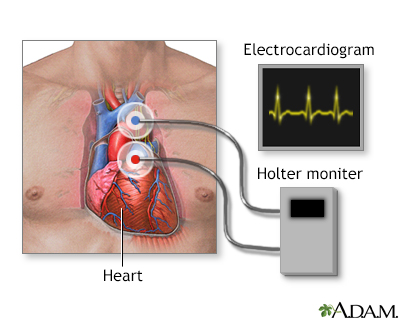 Holter heart monit...
Holter heart monit...
