Pregnancy SmartSiteTM
Crohn's disease; Inflammatory bowel disease - Crohn's disease; Regional enteritis; Ileitis; Granulomatous ileocolitis; IBD - Crohn disease DefinitionCrohn disease is a disease where parts of the digestive tract become inflamed.
Crohn disease is a form of inflammatory bowel disease (IBD). Ulcerative colitis is another form of IBD. 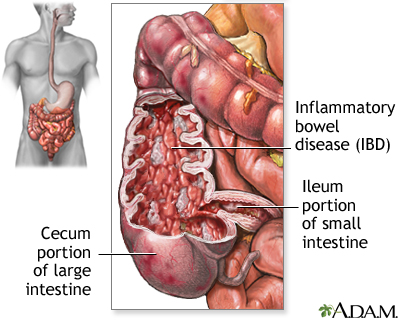 CausesThe exact cause of Crohn disease is unknown. It occurs when your body's immune system mistakenly attacks and destroys healthy body tissue (autoimmune disorder), mainly in the digestive tract. When parts of the digestive tract remain swollen or inflamed, the walls of the intestines become thickened. Factors that may play a role in Crohn disease include:
Crohn disease may occur at any age. It mostly begins in people between ages 15 and 35. But recently Crohn disease has been increasing in the older population, too. SymptomsSymptoms depend on the part of the digestive tract involved. Symptoms range from mild to severe, and can come and go, with periods of flare-ups. The main symptoms of Crohn disease are:
Other symptoms may include:
 Exams and TestsA physical exam may show a mass or tenderness in the abdomen, skin rash, swollen joints, or mouth ulcers. Tests to diagnose Crohn disease include:
A stool culture or other tests may be done to check for other possible causes of the symptoms, such as infection, and to look for inflammation. This disease may also alter the results of the following tests:
TreatmentTips for managing Crohn disease at home: DIET AND NUTRITION You should eat a well-balanced, healthy diet. Include enough calories, protein, and nutrients from a variety of food groups. An elemental diet has been shown to improve Crohn disease and its symptoms. However, this diet is not used often because of the taste. Depending on the location(s) of your Crohn disease, the type of your Crohn disease, and the other problems it may cause, certain foods may be more difficult to eat. Types of food problems may vary from person to person. Some foods can make diarrhea and gas worse. To help ease symptoms, try:
Ask your health care provider about extra vitamins and minerals you may need, such as:
If you have an ileostomy, you will need to learn: STRESS You may feel worried, embarrassed, or even sad and depressed about having a bowel disease. Other stressful events in your life, such as moving, a job loss, or the loss of a loved one can worsen digestive problems. Ask your provider for tips on how to manage your stress. MEDICINES Ask your provider about taking anti-diarrheal medicines. In general, these should be avoided in people with IBD, if possible. Treating the IBD is the key to making diarrhea and other symptoms better. Other medicines to help with symptoms include:
Your provider may also prescribe medicines to help control Crohn disease:
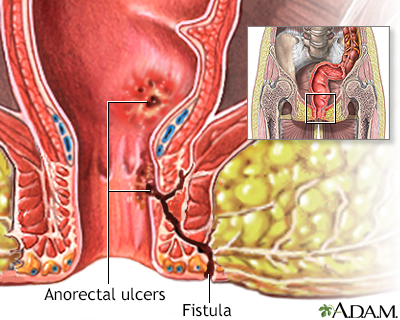
SURGERY Some people with Crohn disease may need surgery to remove a damaged or diseased part of the intestine. In some cases, the entire large intestine is removed, with or without the rectum. People who have Crohn disease that does not respond to medicines may need surgery to treat problems such as:
Surgeries that may be done include:
Support GroupsSocial support can often help with the stress of dealing with illness, and support group members may also have useful tips for finding the best treatment and coping with the condition. More information and support for people with Crohn disease and their families can be found at: www.crohnscolitisfoundation.org Outlook (Prognosis)There is no cure for Crohn disease. However, the goals of treatment are to quiet the disease and keep it quiet. Surgery is used in particular situations but does not cure Crohn disease. If you smoke, stopping will help improve the disease. Possible ComplicationsYou have more risk for small bowel and colon cancer if you have Crohn disease. Your provider may suggest tests to screen for colon cancer. A colonoscopy is often recommended if you have had Crohn disease involving the colon for 8 or more years. Those with more severe Crohn disease may have these problems:
When to Contact a Medical ProfessionalContact your provider if you:
ReferencesAnanthakrishnan AN, Reguerio MD. Management of inflammatory bowel diseases. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 116. Feuerstein JD, Ho EY; American Gastroenterological Association Institute Clinical Guidelines Committee, et al. AGA clinical practice guidelines on the medical management of moderate to severe luminal and perianal fistulizing Crohn's disease. Gastroenterology. 2021;160(7):2496-2508. PMID: 34051983 pubmed.ncbi.nlm.nih.gov/34051983/. Galandiuk S, Netz U, Morpurgo E, Tosato SM, Abu-Freha N, Ellis CT. Colon and rectum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 52. Kaplan GG, Ng SC. Epidemiology, pathogenesis, and diagnosis of inflammatory bowel diseases. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 115. Lichtenstein GR. Inflammatory bowel disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 127. Ricci JP, Talamini MA. Management of Crohn's disease of the small bowel. In: Cameron J, ed. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:134-137. | |
| |
Review Date: 1/24/2025 Reviewed By: Jenifer K. Lehrer, MD, Gastroenterologist, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

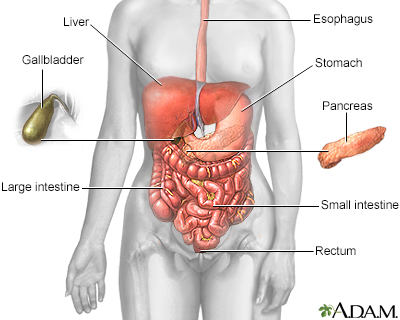 Digestive system
Digestive system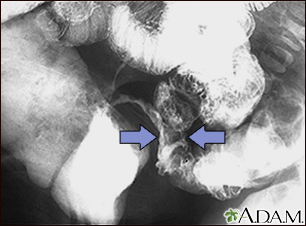 Crohn disease - X-...
Crohn disease - X-...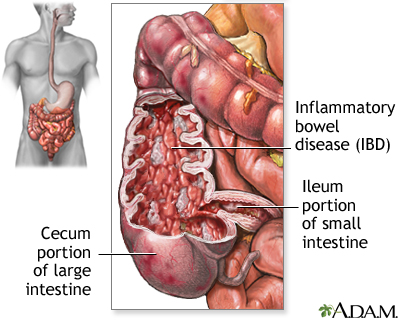 Inflammatory bowel...
Inflammatory bowel...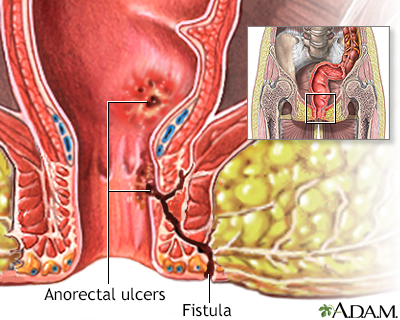 Anorectal fistulas
Anorectal fistulas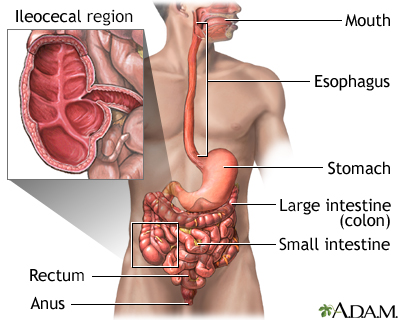 Crohn disease - af...
Crohn disease - af...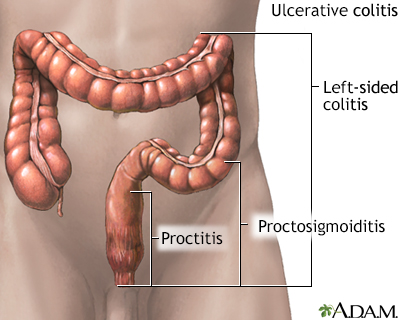 Ulcerative colitis
Ulcerative colitis
