Pregnancy SmartSiteTM
Primary intestinal pseudo-obstruction; Acute colonic ileus; Colonic pseudo-obstruction; Idiopathic intestinal pseudo-obstruction; Ogilvie syndrome; Chronic intestinal pseudo-obstruction; Paralytic ileus - pseudo-obstruction DefinitionIntestinal pseudo-obstruction is a condition in which there are symptoms of blockage of the intestine (bowels) without any physical blockage. CausesIn intestinal pseudo-obstruction, the intestine does not contract and push food, stool, and air through the digestive tract. The chronic disorder most often affects the small intestine, but can also occur in the large intestine (colon). The acute disorder usually affects the large intestine. The condition may start suddenly or be a chronic or long-term problem. Sudden onset is called acute intestinal pseudo-obstruction and usually affects the small intestine and often other parts of the digestive tract. Chronic intestinal pseudo-obstruction usually affects the large intestine (colon.) It is most common in children and older people. The cause of the problem is often unknown. However, problems with the bowel's muscles or nerves may be a cause. Risk factors include:
SymptomsSymptoms include:
Exams and TestsDuring a physical exam, the health care provider will most often see abdominal bloating. Tests include:
TreatmentThe following treatments may be tried:
In severe cases, surgery may be needed. Outlook (Prognosis)Most cases of acute pseudo-obstruction get better in a few days with treatment. In chronic forms of the disease, symptoms can come back and get worse over many years. If the intestine dilates severely, a hole in the bowel (perforation) may occur and surgical removal of the involved bowel may be needed. This may result in an ostomy (attaching the bowel to the abdomen and stool passes into a bag. If malnutrition happens, you may need to be fed through a tube or the vein. Other parts of the GI tract may also have problems from poor contraction. Possible ComplicationsComplications may include:
When to Contact a Medical ProfessionalContact your provider if you have abdominal pain that does not go away or other symptoms of this disorder. ReferencesCamilleri M. Disorders of gastrointestinal motility. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 122. Rayner CK, Hughes PA. Small intestinal motor and sensory function and dysfunction. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 99. | |
| |
Review Date: 5/14/2024 Reviewed By: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

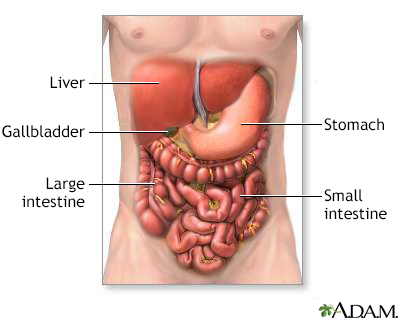 Digestive system o...
Digestive system o...
