Liver cirrhosis - varices; Cryptogenic chronic liver disease - varices; End-stage liver disease - varices; Alcoholic liver disease - varices; NASH varices; Alcoholic hepatitis - varices; Metabolic dysfunction-associated steatohepatitis (MASH) varices DefinitionThe esophagus (food pipe) is the tube that connects your throat to your stomach. Varices are enlarged veins that may be found in the esophagus in people with cirrhosis of the liver. These veins may rupture and bleed. CausesScarring (cirrhosis) of the liver is the most common cause of esophageal varices. This scarring cuts down on blood flowing through the liver. As a result, more blood flows through the veins of the esophagus. The extra blood flow causes the veins in the esophagus to balloon outward forming esophageal varices. Heavy bleeding can occur if the varices tear. Any type of long-term (chronic) liver disease can cause esophageal varices. Varices can also occur in the upper part of the stomach. These are called gastric varices. SymptomsPeople with chronic liver disease and esophageal varices may have no symptoms. If there is only a small amount of bleeding, the only symptom may be dark or black streaks in the stools. If larger amounts of bleeding occur, symptoms may include:
Exams and TestsYour health care provider will do a physical exam which may show:
Tests to find the source of the bleeding and check if there is active bleeding include:
Some providers suggest EGD for people who are newly diagnosed with mild to moderate cirrhosis. This test screens for esophageal varices and treats them before there is bleeding. TreatmentThe goal of treatment is to stop acute bleeding as soon as possible. Bleeding must be controlled quickly to prevent shock and death. If massive bleeding occurs, a person may need to be put on a ventilator to protect their airway and prevent blood from going down into the lungs. To stop the bleeding, the provider may pass an endoscope (tube with a small light at the end) into the esophagus:
Other treatments to stop the bleeding:
Once the bleeding is stopped, other varices can be treated with medicines and medical procedures to prevent future bleeding. These include:
In rare cases, emergency surgery may be used to treat people if other treatment fails. Portacaval shunts or surgery to reduce the pressure in the esophageal varices are treatment options, but these procedures are risky. People with bleeding varices from liver disease may need more treatment for their liver disease, including a liver transplant. Outlook (Prognosis)Bleeding often comes back with or without treatment. Bleeding esophageal varices are a serious complication of liver disease and have a poor outcome. Placement of a shunt can lead to an increase of metabolic toxins gong to the brain. This can lead to mental status changes. Possible ComplicationsFuture problems caused by varices may include:
When to Contact a Medical ProfessionalContact your provider or go to an emergency room if you vomit blood or have black tarry stools. PreventionTreating the causes of liver disease may prevent bleeding. Liver transplantation should be considered for some people. ReferencesGarcia-Tsao G. Cirrhosis and its sequelae. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 139. Savides TJ, Jensen DM. Gastrointestinal bleeding. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 20. Shah VH, Kamath PS. Portal hypertension and variceal bleeding. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 92. | |
| |
Review Date: 12/31/2023 Reviewed By: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |
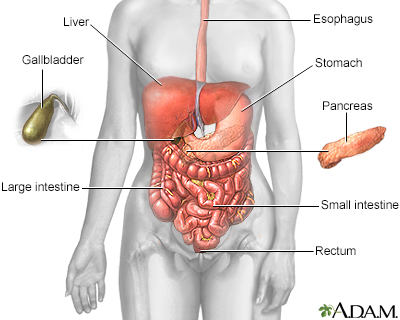 Digestive system
Digestive system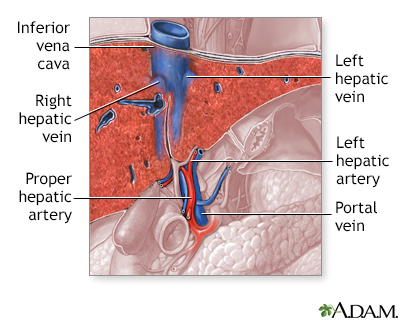 Liver blood supply
Liver blood supply
