Pregnancy SmartSiteTM
Primary liver cell carcinoma; Tumor - liver; Cancer - liver; Hepatoma DefinitionHepatocellular carcinoma is cancer that starts in the liver. CausesHepatocellular carcinoma is the most common type of liver cancer. It occurs more often in men than women. It is most often diagnosed in people age 50 or older. Hepatocellular carcinoma is not the same as metastatic liver cancer. Metastatic liver cancer starts in another organ (such as the breast or colon) and spreads to the liver. In most cases, the cause of hepatocellular liver cancer is long-term damage and scarring of the liver (cirrhosis). Cirrhosis may be caused by:
People with hepatitis B or C are at high risk for liver cancer, even if they do not develop cirrhosis. SymptomsSymptoms of liver cancer may include any of the following:
Exams and TestsYour health care provider will perform a physical exam and ask about your symptoms. The physical exam may show an enlarged, tender liver or other signs of cirrhosis. If your provider suspects liver cancer, tests that may be ordered include:
Some people at risk for liver cancer may get regular blood tests and ultrasounds to see if tumors are developing. TreatmentThe treatment depends on how advanced the cancer is. Surgery may be done if the tumor has not spread. Occasionally the tumor can be treated directly by a procedure known as embolization. This can be done by injecting radiation pellets or chemotherapy directly into the tumor via the blood vessels that feed the tumor. This can sometimes be done prior to surgery or as a procedure by itself. Radiation treatments in the area of the cancer may also be helpful. Ablation is another method that may be used. Ablate means to destroy. Types of ablation include using:
A liver transplant may be recommended. If the cancer can't be surgically removed or has spread outside the liver, there is usually no chance for long-term cure. Treatment instead focuses on improving and extending the person's life. Treatment in this case may use targeted therapy with medicines that can be taken as pills. Newer immunotherapy medicines may also be used and are now the most common forms of treatment for advanced liver cancer. Support GroupsYou can ease the stress of illness by joining a cancer support group. Sharing with others who have common experiences and problems can help you not feel alone. Outlook (Prognosis)If the cancer can't be completely treated, the disease is usually fatal. But survival can vary, depending on how advanced the cancer is and how successful treatment is. When to Contact a Medical ProfessionalContact your provider if you develop ongoing abdominal pain, especially if you have a history of liver disease. PreventionPreventive measures include:
ReferencesAbou-Alfa GK, Jarnagin W, El Dika I, et al. Liver and bile duct cancer. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 77. Di Bisceglie AM, Befeler AS. Hepatic tumors and cysts. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 96. National Cancer Institute website. Primary liver cancer treatment (PDQ®)–health professional version. www.cancer.gov/types/liver/hp/adult-liver-treatment-pdq. Updated April 17, 2025. Accessed July 18, 2025. National Comprehensive Cancer Network website. NCCN clinical practice guidelines in oncology: hepatocellular carcinoma. Version 1.2025. www.nccn.org/professionals/physician_gls/pdf/hcc.pdf. Updated March 20, 2025. Accessed July 18, 2025. | |
| |
Review Date: 7/9/2025 Reviewed By: Warren Brenner, MD, Oncologist, Lynn Cancer Institute, Boca Raton, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

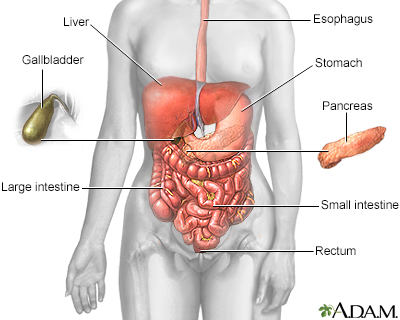 Digestive system
Digestive system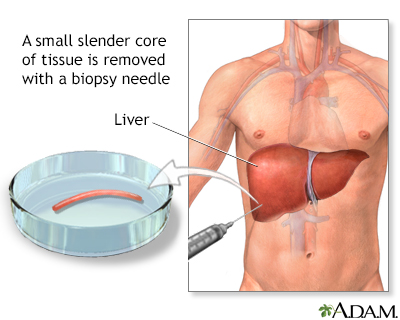 Liver biopsy
Liver biopsy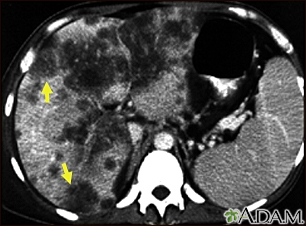 Hepatocellular can...
Hepatocellular can...
