Pregnancy SmartSiteTM
Periodic paralysis - hyperkalemic; Familial hyperkalemic periodic paralysis; HyperKPP; HyperPP; Gamstorp disease; Potassium-sensitive periodic paralysis DefinitionHyperkalemic periodic paralysis (hyperPP) is a disorder that causes occasional episodes of muscle weakness and sometimes a higher than normal level of potassium in the blood. The medical name for high potassium level is hyperkalemia. HyperPP is one of a group of genetic disorders that includes hypokalemic periodic paralysis and thyrotoxic periodic paralysis. CausesHyperPP is congenital. This means it is present at birth. In most cases, it is passed down through families (inherited) as an autosomal dominant disorder. In other words, only one parent needs to pass the gene related to this condition on to their child in order for the child to be affected. Occasionally, the condition may be the result of a genetic problem that is not inherited. It is believed that the disorder is related to problems with the way the body controls sodium and potassium levels in cells. Risk factors include having other family members with periodic paralysis. It affects men and women equally. SymptomsSymptoms include attacks of muscle weakness or loss of muscle movement (paralysis) that come and go. There is normal muscle strength between attacks. Attacks usually begin in childhood. How often the attacks occur varies. Some people have several attacks a day. They are usually not severe enough to need therapy. Some people have associated myotonia, in which they cannot immediately relax their muscles after use. The weakness or paralysis:
Triggers may include:
Exams and TestsThe health care provider may suspect hyperPP based on a family history of the disorder. Other clues to the disorder are muscle weakness symptoms that come and go with normal or high results of a blood potassium test. Between attacks, a physical examination shows nothing abnormal. During and between attacks, the potassium blood level can be normal or high. During an attack, muscle reflexes are decreased or absent. And muscles go limp rather than staying stiff. Muscle groups near the body, such as the shoulders and hips, are involved more often than the arms and legs. Tests that may done include:
Other tests may be ordered to rule out other causes. TreatmentThe goal of treatment is to relieve symptoms and prevent further attacks. Attacks are seldom severe enough to require emergency treatment. But irregular heartbeats (heart arrhythmias) may also occur during attacks, for which emergency treatment is needed. Muscle weakness can become worse with repeated attacks, so treatment to prevent the attacks should occur as soon as possible. Glucose or other carbohydrates (sugars) given during an attack may reduce the severity of the symptoms. Calcium or diuretics may need to be given through a vein to stop sudden attacks. Outlook (Prognosis)Sometimes, attacks disappear later in life on their own. But repeated attacks may lead to permanent muscle weakness. HyperPP responds well to treatment. Treatment may prevent, and may even reverse, progressive muscle weakness. Possible ComplicationsHealth problems that may be due to hyperPP include:
When to Contact a Medical ProfessionalContact your provider if you or your child has muscle weakness that comes and goes, especially if you have family members who have periodic paralysis. Go to the emergency room or call the local emergency number (such as 911) if you faint or have difficulty breathing, speaking, or swallowing. PreventionThe medicines acetazolamide and thiazides prevent attacks in many cases. A low potassium, high carbohydrate diet, and light exercise may help prevent attacks. Avoiding fasting, strenuous activity, or cold temperatures also may help. ReferencesBoegle AK, Narayanaswami P. Treatment and management of disorders of neuromuscular hyperexcitability and periodic paralysis. In: Bertorini TE, ed. Neuromuscular Disorders: Treatment and Management. 2nd ed. St Louis, MO: Elsevier; 2022:chap 18. Doughty CT, Amato AA. Disorders of skeletal muscle. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff’s Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 109. Kang MK, Kerchner GA, Ptacek LJ. Channelopathies: episodic and electrical disorders of the nervous system. In: Jankovic J, Mazziotta JC, Pomeroy SK, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 98. Weimer M, Reese JJ, Tilton AH. Acute neuromuscular diseases and disorders. In: Zimmerman JJ, Clark RSB, Fuhrman BP, et al. Fuhrman and Zimmerman's Pediatric Critical Care. 6th ed. Philadelphia, PA: Elsevier; 2022:chap 68. | |
| |
Review Date: 12/31/2023 Reviewed By: Walead Latif, MD, Nephrologist and Clinical Associate Professor, Rutgers Medical School, Newark, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

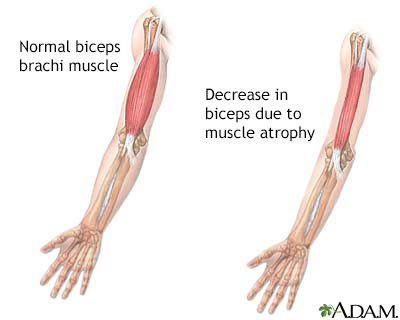 Muscular atrophy
Muscular atrophy
