Pregnancy SmartSiteTM
Keratitis sicca; Xerophthalmia; Keratoconjunctivitis sicca DefinitionYou need tears to moisten your eyes and to wash away particles that have gotten into your eyes. A healthy tear film on the eye is necessary for good vision. Dry eyes develop when the eye is unable to maintain a healthy coating of tears. CausesDry eye syndrome commonly occurs in people who are otherwise healthy. It becomes more common with older age. This can occur due to hormonal changes that make your eyes produce fewer tears. Dry eye syndrome is sometimes caused or worsened by a condition called meibomianitis, which changes the normal tear film. Other common causes of dry eyes include:
Dry eye syndrome can also be caused by:
SymptomsSymptoms may include:
Exams and TestsTests may include:
TreatmentThe first step in treatment is artificial tears. These come as preserved (screw cap bottle) and unpreserved (twist open vial or multidose bottle). Preserved tears are more convenient, but some people are sensitive to preservatives. There are many brands available without a prescription. Start using the drops at least 2 to 4 times per day. If your symptoms are not better after a couple of weeks of regular use:
Other treatments for dry eyes may include:
Other helpful steps include:
Some dry eye symptoms are due to sleeping with the eyes slightly open. Lubricating ointments work best for this problem. You should use them only in small amounts since they can blur your vision. It is best to use them before sleep. Surgery may be helpful if symptoms are because the eyelids are in an abnormal position. Outlook (Prognosis)Most people with dry eye syndrome have only discomfort, and no vision loss. Possible ComplicationsIn severe cases, the clear covering on the eye (cornea) may become damaged or infected. When to Contact a Medical ProfessionalContact your provider right away if:
PreventionStay away from dry environments and things that irritate your eyes to help prevent symptoms. ReferencesBrissette AR, Bohm KJ, Starr CE. Dry eye overview: classification and treatment overview. In: Mannis MJ, Holland EJ, eds. Cornea. 5th ed. Philadelphia, PA: Elsevier; 2022:chap 31. Dhawlikar NS, Holdstein MH, Rao NK. Dry eye disease. In: Yanoff M, Duker JS, eds. Ophthalmology. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 4.23 Jeang LA. Dry eye syndrome. In: Kellerman RD, Rakel DP, Heidelbaugh JJ, Lee EM, eds. Conn's Current Therapy 2024. Philadelphia, PA: Elsevier; 2024:527-529. | |
| |
Review Date: 10/2/2024 Reviewed By: Audrey Tai, DO, MS, Athena Eye Care, Mission Viejo, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

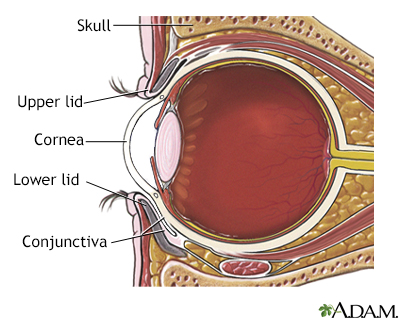 Eye anatomy
Eye anatomy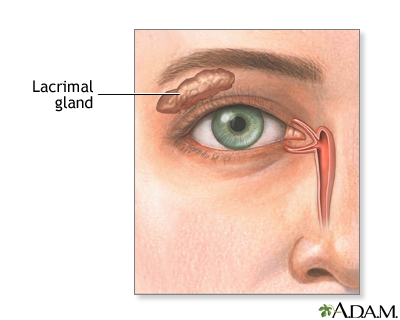 Lacrimal gland
Lacrimal gland
