Pregnancy SmartSiteTM
Cystitis - interstitial; IC DefinitionInterstitial cystitis (IC) is a long-term (chronic) problem in which pain, pressure, or burning is present in the bladder. It is often associated with urinary frequency or urgency. It is also called painful bladder syndrome. CausesThe bladder is a hollow organ that stores urine. It has a thin layer of muscle inside it. When your bladder fills up with urine, it sends a signal to your brain, telling the muscles to squeeze. Under normal conditions, these signals are not painful. If you have interstitial cystitis, the signals from the bladder are painful and may occur even when the bladder is not full. The condition most often occurs between ages 20 to 40, although it has been reported in younger people. Women are 10 times more likely to have IC than men. The exact cause of this condition is unknown. SymptomsSymptoms of IC are chronic. Symptoms tend to come and go with periods of lesser or worse severity. Common symptoms include:
Many people who have long-term IC may also have other conditions such as endometriosis, fibromyalgia, irritable bowel syndrome, other chronic pain syndromes, anxiety, or depression. Exams and TestsYour health care provider will look for other causes of your symptoms. These include:
Tests are done on your urine to look for infection or cells that suggest cancer inside the bladder. During a cystoscopy, the provider uses a special tube with a small camera on the end to look inside your bladder. A sample or biopsy of the lining of your bladder may be taken. Tests at your provider's office may also be done to show how well your bladder fills and how well it empties. TreatmentThere is no cure for IC, and there are no standard treatments. Treatment is based on trial and error until you find relief. Results vary from person to person. DIET AND LIFESTYLE CHANGES Some people find that making changes in their diet can help control symptoms. Try to avoid foods and beverages that can cause bladder irritation. Stop eating certain foods, one at a time, to see if your symptoms get better. Reduce or stop consuming caffeine, chocolate, carbonated beverages, citrus drinks, and spicy or acidic foods (such as those with high levels of vitamin C). Other foods that the Interstitial Cystitis Association lists as possibly causing bladder irritation are:
You and your provider should discuss methods you can use for bladder training. These may include training yourself to urinate at specific times or using pelvic floor physical therapy and biofeedback to relieve pelvic floor muscle tension and spasms. MEDICINES AND PROCEDURES Combination therapy may include medicines such as:
Other therapies include:
Support GroupsMore information and support for people with interstitial cystitis and their families can be found at: Interstitial Cystitis Association: www.ichelp.org/get-involved/join-the-ic-community/ and others. Outlook (Prognosis)Treatment results vary. Some people respond well to simple treatments and dietary changes. Others may require extensive treatments or surgery. When to Contact a Medical ProfessionalContact your provider if you have symptoms of IC. Be sure to mention that you suspect this disorder. It is not always easily recognized or diagnosed. It is often confused with having repeated urinary tract infection. ReferencesClemens JQ, Erickson DR, Varela NP, Lai HH. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol. 2022;208(1):34-42. PMID: 35536143 pubmed.ncbi.nlm.nih.gov/35536143/. Grochmal SA. Office testing and treatment options for interstitial cystitis (painful bladder syndrome). In: Fowler GC, ed. Pfenninger and Fowler's Procedures for Primary Care. 4th ed. Philadelphia, PA: Elsevier; 2020:chap 98. Lentz GM, Miller JL. Lower urinary tract function and disorders: physiology of micturition, voiding dysfunction, urinary incontinence, urinary tract infections, and painful bladder syndrome. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 21. Moldwin RM, Hanno PM. Interstitial cystitis/bladder pain syndrome and related disorders. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 57. | |
| |
Review Date: 4/1/2025 Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

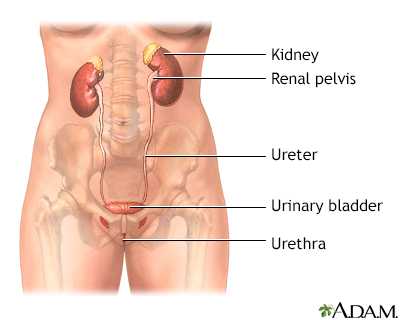 Female urinary tra...
Female urinary tra...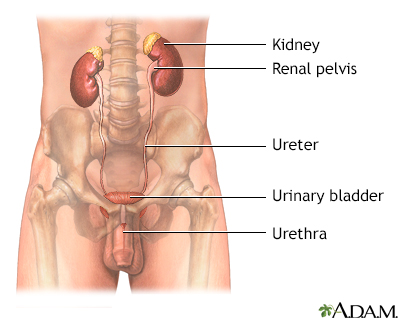 Male urinary tract
Male urinary tract
