Pregnancy SmartSiteTM
NBP; Prostatodynia; Pelvic pain syndrome; CPPS; Chronic nonbacterial prostatitis; Chronic genitourinary pain DefinitionChronic nonbacterial prostatitis causes long-term pain and urinary symptoms. It involves the prostate gland or other parts of a man's lower urinary tract or genital area. This condition is not caused by an infection with bacteria. CausesPossible causes of nonbacterial prostatitis include:
Life stresses and emotional factors may play a part in the problem. Most men with chronic prostatitis have the nonbacterial form. SymptomsSymptoms may include:
Exams and TestsMost of the time, a physical exam is normal. However, the prostate may be swollen or tender. Urine tests may show white or red blood cells in the urine. A semen analysis may show a higher number of white blood cells and low sperm count with poor movement. Urine culture or culture from the prostate does not show bacteria. TreatmentTreatment for nonbacterial prostatitis is difficult. The problem is hard to cure, so the main goal is to control symptoms. Several types of medicines may be used to treat the condition. These include:
Some people have found some relief from pollen extract (Cernitin) and allopurinol. But research does not confirm their benefit for large numbers of men. Stool softeners may help reduce discomfort with bowel movements. Surgery, called transurethral resection of the prostate, may be done in rare cases if medicine does not help. In most cases, this surgery is not done on younger men. It may cause retrograde ejaculation. The surgery can lead to sterility, impotence, and incontinence. Other treatments that may be tried include:
Outlook (Prognosis)Many people respond to treatment. However, others do not get relief, even after trying many things. Symptoms often come back and may not be treatable. Possible ComplicationsUntreated symptoms of nonbacterial prostatitis may lead to sexual and urinary problems. These problems can affect your lifestyle and emotional well-being. When to Contact a Medical ProfessionalContact your health care provider if you have symptoms of prostatitis. ReferencesDouglass L, Pontari M. Inflammatory and pain conditions of the lower genitourinary tract: prostatitis and related pain conditions, orchitis, and epididymitis. In: Dmochowski RR, Kavoussi LR, Peters CA, et al, eds. Campbell-Walsh-Wein Urology. 13th ed. Philadelphia, PA: Elsevier; 2026:chap 27. Kaplan SA. Benign prostatic hyperplasia and prostatitis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 114. McGowan CC. Prostatitis, epididymitis, and orchitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 110. US Department of Health and Human Services; National Institute of Diabetes and Digestive and Kidney Diseases website. Prostatitis: inflammation of the prostate. www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostatitis-inflammation-prostate. Updated July 2014. Accessed July 3, 2025. | |
| |
Review Date: 7/1/2025 Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

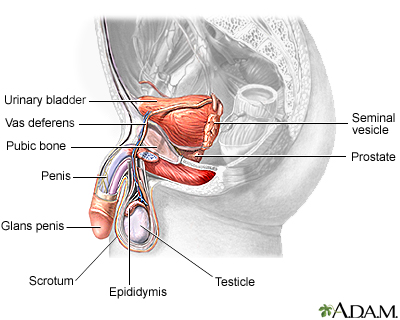 Male reproductive ...
Male reproductive ...
