Pregnancy SmartSiteTM
Neonatal polycythemia; Hyperviscosity - newborn DefinitionPolycythemia means there are too many red blood cells (RBCs) in an infant's blood. CausesThe percentage of RBCs in the infant's blood is called the "hematocrit." When this is greater than 65%, polycythemia is present. Polycythemia can result from conditions that develop before birth. These may include:
The extra RBCs can slow or block the flow of blood in the smallest blood vessels. This is called hyperviscosity. This may lead to tissue death from lack of oxygen. This blocked blood flow can affect all organs, including the kidneys, lungs, and brain. SymptomsSymptoms may include:
Exams and TestsThere may be signs of breathing problems, kidney failure, low blood sugar, or newborn jaundice. If the baby has symptoms of hyperviscosity, a blood test to count the number of RBCs will be done. This test is called a hematocrit. Other tests may include:
TreatmentThe baby will be monitored for complications of hyperviscosity. Fluids may be given through the vein. A partial volume exchange transfusion is sometimes still done in some cases. However, there is little evidence that this is effective. It is most important to treat the underlying cause of the polycythemia. Outlook (Prognosis)The outlook is good for infants with mild hyperviscosity. Good results are also possible in infants who receive treatment for severe hyperviscosity. The outlook will depend largely on the reason for the condition. Some children may have mild developmental changes. Parents should contact their health care provider if they think their child shows signs of delayed development. Possible ComplicationsComplications may include:
ReferencesOwusu-Ansah A, Letterio J, Ahuja SP. Red blood cell disorders in the fetus and neonate. In: Martin RJ, Fanaroff AA, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 81. Tashi T, Prchal JT. Primary and secondary erythrocytosis. In: Fish JD, Lipton JM, Lanzkowsky P, eds. Lanzkowsky's Manual of Pediatric Hematology and Oncology. 7th ed. Cambridge, MA: Elsevier Academic Press; 2022:chap 10. Thom CS, Lambert MP. Blood disorders. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 138. | |
| |
Review Date: 4/6/2025 Reviewed By: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

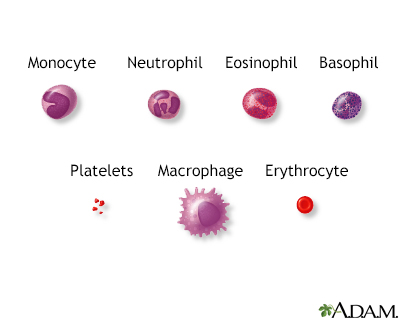 Blood cells
Blood cells
