Pregnancy SmartSiteTM
DefinitionCryoglobulinemia is the presence of abnormal proteins in the blood. These proteins thicken in cold temperatures. CausesCryoglobulins are antibodies. It is not yet known why they become solid or gel-like at low temperatures in the laboratory. In the body, these antibodies can form immune complexes that can cause inflammation and block blood vessels. This is called cryoglobulinemic vasculitis. This may lead to problems ranging from skin rashes to kidney failure. Cryoglobulinemia is part of a group of diseases that cause damage and inflammation of the blood vessels throughout the body (vasculitis). There are three main types of this condition. They are grouped based on the type of antibody that is produced:
Type I cryoglobulinemia is most often related to cancer of the blood or immune systems. Types II and III are also referred to as mixed cryoglobulinemia. Types II and III are most often found in people who have a long-lasting (chronic) inflammatory condition, such as an autoimmune disease or hepatitis C. Most people with the type II form of cryoglobulinemia have a chronic hepatitis C infection. Other conditions that may be related to cryoglobulinemia include:
SymptomsSymptoms will vary, depending on the type of disorder you have and the organs that are involved. Symptoms may include:
Exams and TestsThe health care provider will do a physical exam. You will be checked for signs of liver and spleen swelling. Tests for cryoglobulinemia include:
Other tests may include:
TreatmentMIXED CRYOGLOBULINEMIA (TYPES II AND III) Mild or moderate forms of cryoglobulinemia can often be treated by taking steps to deal with the underlying cause. Current direct-acting medicines for hepatitis C eliminate the virus in nearly all people. As hepatitis C goes away, the cryoglobulins will disappear in about one half of all people over the next 12 months. Your provider will continue to monitor the cryoglobulins after treatment. Severe cryoglobulinemia vasculitis involves vital organs or large areas of skin. It is treated with corticosteroids and other medicines that suppress the immune system.
TYPE I CRYOGLOBULINEMIA This disorder is due to a cancer of the blood or immune system such as multiple myeloma. Treatment is directed against the abnormal cancer cells that produce the cryoglobulin. Outlook (Prognosis)Most of the time, mixed cryoglobulinemia does not lead to death. Outlook can be poor if the kidneys are affected. Possible ComplicationsComplications include:
When to Contact a Medical ProfessionalContact your provider if:
PreventionThere is no known prevention for the condition.
ReferencesDe Vita S, Gandolfo S, Quartuccio L. Cryoglobulinemia. In: Hochberg MC, Gravallese EM, Smolen JS, van der Heijde D, Weinblatt ME, Weisman MH, eds. Rheumatology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 171. McPherson RA, Riley RS, Massey HD. Laboratory evaluation of immunoglobulin function and humoral immunity. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 24th ed. Philadelphia, PA: Elsevier; 2022:chap 47. Rajkumar SV. Plasma cell disorders. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 173. Stone JH. Immune complex-mediated small-vessel vasculitis. In: Firestein GS, McInnes IB, Koretzky GA, Mikuls TR, Neogi T, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 92. | |
| |
Review Date: 1/28/2025 Reviewed By: Diane M. Horowitz, MD, Rheumatology and Internal Medicine, Northwell Health, Great Neck, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Cryoglobulinemia o...
Cryoglobulinemia o...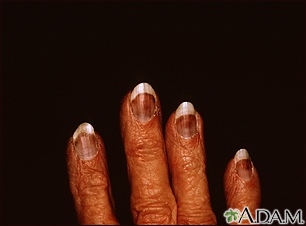 Cryoglobulinemia -...
Cryoglobulinemia -...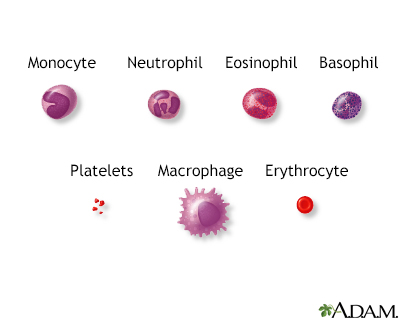 Blood cells
Blood cells
