Pregnancy SmartSiteTM
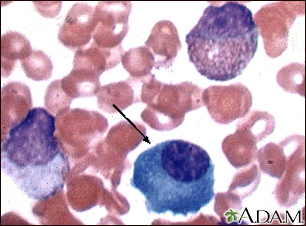
Waldenström macroglobulinemia; Macroglobulinemia - primary; Lymphoplasmacytic lymphoma; Monoclonal macroglobulinemia; Waldenström macroglobulinemia DefinitionWaldenström macroglobulinemia (WM) is a cancer of the B lymphocytes (a type of white blood cell). WM is associated with the overproduction of proteins called IgM antibodies. CausesWM is a result of a condition called lymphoplasmacytic lymphoma. This is a cancer of the white blood cells, in which the B immune cells start dividing rapidly. The exact cause of too much production of the IgM antibody is unknown. Hepatitis C may increase the risk of WM. Gene mutations are often found in the malignant B cells. Production of excess IgM antibodies can cause several types of problems:
WM is very rare. Most people with this condition are over 65 years of age. SymptomsSymptoms of WM may include any of the following:
Exams and TestsA physical exam may reveal a swollen spleen, liver, and lymph nodes. An eye exam may show enlarged veins in the retina or retinal bleeding (hemorrhages). A complete blood count (CBC) may show a low number of red blood cells or platelets. Blood chemistry may show evidence of kidney disease. A blood test called serum protein electrophoresis shows an increased level of the IgM antibody. Levels are often higher than 3000 milligrams per deciliter (mg/dL), or 30 grams per liter (g/L). An immunofixation test will be done to show if the IgM antibody is derived from a single cell type (clonal). A serum viscosity test can tell if the blood has become thick. Symptoms usually occur when the blood is four times thicker than normal. A bone marrow biopsy will show increased numbers of abnormal cells that look like both lymphocytes and plasma cells. Additional tests that may be done include:
TreatmentSome people with WM who have increased IgM antibodies do not have symptoms. This condition is known as smoldering WM. No treatment is needed other than careful follow-up. In people with symptoms, treatment aims at decreasing the symptoms and the risk of developing organ damage. There is no current standard treatment. Your health care provider may suggest that you participate in a clinical trial. Plasmapheresis removes IgM antibodies from the blood. It also controls the symptoms caused by blood thickening. Medicines may include corticosteroids, a combination of chemotherapy medicines and the monoclonal antibody to B cells, rituximab. Autologous stem cell transplant may be recommended for some people with otherwise good health. People who have a low number of red or white blood cells or platelets may need transfusions or antibiotics. Outlook (Prognosis)The average survival is about 5 years. Some people live more than 10 years. In some people, the disorder may produce few symptoms and progress slowly. Possible ComplicationsComplications of WM may include:
When to Contact a Medical ProfessionalContact your provider if symptoms of WM develop. ReferencesCastillo JJ, Treon SP. Waldenström macroglobulinemia/lymphoplasmacytic lymphoma. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 92. Kapoor P, Ansell SM, Fonseca R, et al. Diagnosis and management of Waldenström macroglobulinemia: Mayo stratification of macroglobulinemia and risk-adapted therapy (mSMART) guidelines 2016. JAMA Oncol. 2017;3(9):1257-1265. PMID: 28056114 pubmed.ncbi.nlm.nih.gov/28056114/. Rajkumar SV. Plasma cell disorders. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 173. | |
| |
Review Date: 5/9/2024 Reviewed By: Neil J. Gonter, MD, Assistant Professor of Medicine, Columbia University, NY and private practice specializing in Rheumatology at Rheumatology Associates of North Jersey, Teaneck, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Waldenstroms
Waldenstroms Antibodies
Antibodies
