Pregnancy SmartSiteTM
Soft chancre; Ulcus molle; Sexually transmitted disease - chancroid; STD - chancroid; Sexually transmitted infection - chancroid; STI - chancroid DefinitionChancroid is a bacterial infection that is spread through sexual contact. CausesChancroid is caused by a bacterium called Haemophilus ducreyi. The infection is found in many parts of the world, such as Africa and southwest Asia. The infection is uncommon in the United States. Most people in the United States who are diagnosed with chancroid get it outside the country in areas where the infection is more common. SymptomsWithin 1 day to 2 weeks after becoming infected, a person will get a small bump on the genitals. The bump becomes an ulcer within a day after it first appears. The ulcer:
About one half of infected men have only a single ulcer. Women often have 4 or more ulcers. The ulcers appear in specific locations. Common locations in men are:
In women, the most common location for ulcers is the outer lips of the vagina (labia majora). "Kissing ulcers" may develop. Kissing ulcers are those that occur on opposite surfaces of the labia. Ulcers also may form on the:
The most common symptoms in women are pain with urination and intercourse. The ulcer may look like the sore of primary syphilis (chancre). About one half of the people who are infected with chancroid develop enlarged lymph nodes in the groin. In one half of the people who have swelling of the groin lymph nodes, the nodes break through the skin and cause draining abscesses. The swollen lymph nodes and abscesses are also called buboes. Exams and TestsYour health care provider diagnoses chancroid by:
There is no blood test for chancroid. TreatmentThe infection is treated with antibiotics, including ceftriaxone and azithromycin. Large lymph node swellings may need to be drained, either with a needle or local surgery. Outlook (Prognosis)Chancroid can get better on its own. Some people have months of painful ulcers and drainage. Antibiotic treatment often clears up the lesions quickly with very little scarring. Possible ComplicationsComplications include urethral fistulas and scars on the foreskin of the penis in uncircumcised males. People with chancroid should also be checked for other sexually transmitted infections, including but not limited to syphilis, HIV, and genital herpes. In people with HIV, chancroid may take much longer to heal. When to Contact a Medical ProfessionalContact your provider for an appointment if:
PreventionChancroid is spread by sexual contact with an infected person. Avoiding all forms of sexual activity is the only absolute way to prevent an STI. However, safer sex behaviors may reduce your risk. The proper use of condoms, either the male or female type, greatly decreases the risk of catching an STI. You need to wear the condom from the beginning to the end of each sexual activity. ReferencesEckert LO, Lentz GM. Genital tract infections: vulva, vagina, cervix, toxic shock syndrome, endometritis, and salpingitis. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 23. James WD. Bacterial infections. In: James WD, ed. Andrews' Diseases of the Skin. 14th ed. St Louis, MO: Elsevier; 2026:chap 12. Riesbeck K. Haemophilus species, including H. influenzae and H. ducreyi (chancroid). In: Blaser MJ, Cohen JI, Holland SM, et al, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 10th ed. Philadelphia, PA: Elsevier; 2026:chap 230. Spinola SM. Chancroid. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 276. | |
| |
Review Date: 8/5/2025 Reviewed By: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

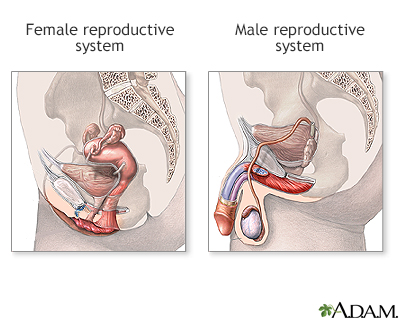 Male and female re...
Male and female re...
