Pregnancy SmartSiteTM
Pseudohypertrophic muscular dystrophy; Muscular dystrophy - Duchenne type DefinitionDuchenne muscular dystrophy is an inherited disorder. It involves muscle weakness, which quickly gets worse. CausesDuchenne muscular dystrophy is a form of muscular dystrophy. It worsens quickly. Other muscular dystrophies (including Becker muscular dystrophy) get worse much more slowly. Duchenne muscular dystrophy is caused by a defective gene for dystrophin (a protein in the muscles). However, it often occurs in people without a known family history of the condition. The condition most often affects boys due to the way the disease is inherited. The sons of women who are carriers of the disease (women with a defective gene, but no symptoms themselves) each have a 50% chance of having the disease. The daughters each have a 50% chance of being carriers. Very rarely, a female can be affected by the disease. Duchenne muscular dystrophy occurs in about 1 out of every 3,600 male infants. Because this is an inherited disorder, risks include a family history of Duchenne muscular dystrophy. SymptomsSymptoms most often appear before age 6. They may start as early as infancy. Most boys show no symptoms in the first few years of life. Symptoms may include:
Muscle weakness:
Progressive difficulty walking:
Exams and TestsA complete nervous system (neurological), heart, lung, and muscle exam may show:
Tests may include:
TreatmentThere is no known cure for Duchenne muscular dystrophy. Treatment aims to control symptoms to improve quality of life. Steroid drugs can slow the loss of muscle strength. They may be started when the child is diagnosed or when muscle strength begins to decline. Other treatments may include:
However, the effects of these treatments have not been proven. Stem cells and gene therapy may be used in the future. Genetic therapies may be helpful to certain patients, depending on the genetic cause. Each therapy only works on a small number of patients, depending on their specific genetic change (mutation). While these treatments have been shown to increase dystrophin production, they have not yet been shown to have significant clinical benefits. Treatments include:
The use of steroids and the lack of physical activity can lead to excessive weight gain. Activity is encouraged. Inactivity (such as bedrest) can make the muscle disease worse. Physical therapy may help to maintain muscle strength and function. Speech therapy is often needed. Other treatments may include:
Several new treatments are being studied in trials. Support GroupsYou can ease the stress of illness by joining a support group where members share common experiences and problems. The Muscular Dystrophy Association is an excellent source of information on this disease. Outlook (Prognosis)Duchenne muscular dystrophy leads to progressively worsening disability. Death often occurs from lung disorders, although advances in supportive care have resulted in many men living to age 35 years. Possible ComplicationsComplications may include:
When to Contact a Medical ProfessionalContact your health care provider if:
PreventionPeople with a family history of the disease may want to seek genetic counseling. Genetic studies done during pregnancy are very accurate in detecting Duchenne muscular dystrophy. ReferencesBharucha-Goebel DX. Muscular dystrophies. In: Kliegman RM, St Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 627. Genetic and Rare Diseases Information Center (GARD). Duchenne muscular dystrophy. rarediseases.info.nih.gov/diseases/6291/duchenne-muscular-dystrophy. Updated June 2024. Accessed June 11, 2024. Lee BH. The Dystrophinopathies. Continuum (Minneap Minn). 2022;28(6):1678-1697. PMID: 36537975 pubmed.ncbi.nlm.nih.gov/36537975/. Muscular Dystrophy Association website. Duchenne muscular dystrophy. www.mda.org/disease/duchenne-muscular-dystrophy. Accessed March 5, 2024. Selcen D. Muscle diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 389. Warner WC, Sawyer JR. Neuromuscular disorders. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 35. | |
| |
Review Date: 12/31/2023 Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 06/11/2024. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

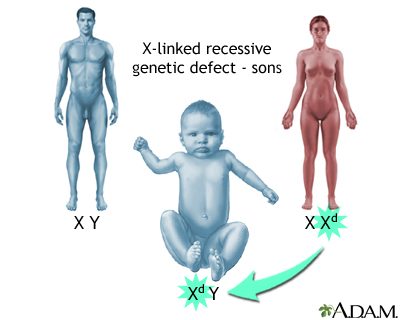 X-linked recessive...
X-linked recessive...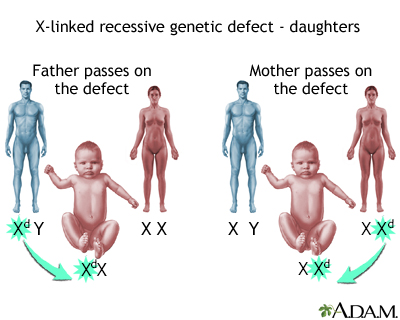 X-linked recessive...
X-linked recessive...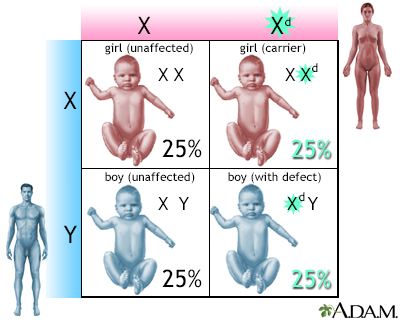 X-linked recessive...
X-linked recessive...
