Pregnancy SmartSiteTM
Oculosympathetic paresis; Horner's syndrome DefinitionHorner syndrome is a rare condition that affects the nerves to the eyes and face. CausesHorner syndrome can be caused by any interruption in a set of nerve fibers that start in the part of the brain called the hypothalamus and travel to the face and eyes. These nerve fibers are involved with sweating, the pupils in your eyes, and the upper and lower eyelid muscles. Damage of the nerve fibers can result from:
In rare cases, Horner syndrome is present at birth. The condition may occur with a lack of color (pigmentation) of the iris (colored part of the eye). SymptomsSymptoms of Horner syndrome may include:
There may also be other symptoms, depending on the location of the affected nerve fiber. These may include:
Exams and TestsYour health care provider will perform a physical exam and ask about the symptoms. An eye exam may show:
Depending on the suspected cause, tests may be done, such as:
You may need to be referred to a provider who specializes in vision problems related to the nervous system (neuro-ophthalmologist). TreatmentTreatment depends on the underlying cause of the condition. There is no treatment for Horner syndrome itself. Ptosis is very mild and in rare cases affects vision in Horner syndrome. This can be corrected by cosmetic surgery or treated with eyedrops. Your provider can tell you more. Outlook (Prognosis)The outcome depends on whether treatment of the cause is successful. Possible ComplicationsThere are no direct complications of Horner syndrome itself. But, there may be complications from the disease that caused Horner syndrome or from its treatment. When to Contact a Medical ProfessionalContact your provider if you have symptoms of Horner syndrome. ReferencesBalcer LJ. Pupillary disorders. In: Liu GT, Volpe NJ, Galetta SL, eds. Liu, Volpe, and Galetta's Neuro-Ophthalmology. 3rd ed. Philadelphia, PA: Elsevier; 2019:chap 13. Tamhankar MA. Eye movement disorders: third, fourth, and sixth nerve palsies and other causes of diplopia and ocular misalignment. In: Liu GT, Volpe NJ, Galetta SL, eds. Liu, Volpe, and Galetta's Neuro-Ophthalmology. 3rd ed. Philadelphia, PA: Elsevier; 2019:chap 15. Thurtell MJ, Rucker JC. Pupillary and eyelid abnormalities. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 17. | |
| |
Review Date: 6/13/2024 Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

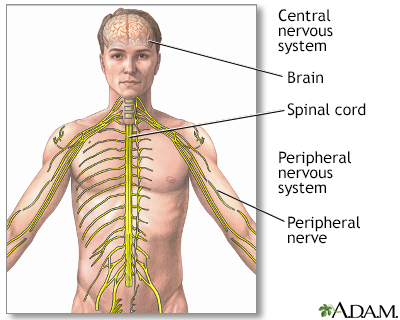 Central nervous sy...
Central nervous sy...
