Pregnancy SmartSiteTM
AVM - cerebral; Arteriovenous hemangioma; Stroke - AVM; Hemorrhagic stroke - AVM DefinitionA cerebral arteriovenous malformation (AVM) is an abnormal connection between the arteries and veins in the brain that usually forms before birth. CausesThe exact cause of cerebral AVM is unknown, however growing evidence suggests a genetic cause. An AVM occurs when arteries in the brain connect directly to nearby veins without having the normal small blood vessels (capillaries) between them. AVMs vary in size and location in the brain. An AVM rupture occurs because of pressure and damage to the blood vessel. This allows blood to leak (hemorrhage) into the brain or surrounding tissues and reduces blood flow to the brain. Cerebral AVMs are rare. Although the condition is present at birth, symptoms may occur at any age. Ruptures happen most often in people ages 15 to 20. It can also occur later in life. Some people with an AVM also have brain aneurysms. SymptomsIn about one half of people with AVMs, the first symptoms are those of a stroke caused by bleeding in the brain. Symptoms of an AVM that is bleeding are:
Symptoms due to pressure on one area of the brain include:
Exams and TestsYour health care provider will perform a physical examination. You'll be asked about your symptoms, with a focus on your nervous system problems. Tests that may be used to diagnose an AVM include:
TreatmentDetermining the best treatment for an AVM that is found on an imaging test, but is not causing any symptoms, can be difficult. Your provider will discuss with you:
Your provider may discuss different factors that may increase your risk for bleeding, including:
A bleeding AVM is a medical emergency. The goal of treatment is to prevent further complications by controlling the bleeding and seizures and, if possible, removing the AVM. Three surgical treatments are available. Some treatments are used together. Open brain surgery removes the abnormal connection. The surgery is done through an opening made in the skull. Embolization (endovascular treatment):
Medicines to stop seizures are prescribed if needed. Outlook (Prognosis)Some people, whose first symptom is excessive brain bleeding, will die. Others may have permanent seizures and brain and nervous system problems. AVMs that do not cause symptoms by the time people reach their late 40s or early 50s are more likely to remain stable, and in rare cases, cause symptoms. Only in rare cases will they cause symptoms. Possible ComplicationsComplications may include:
Possible complications of open brain surgery include:
When to Contact a Medical ProfessionalGo to the emergency room or call 911 or the local emergency number if you have:
Also seek medical attention right away if you have a first-time seizure, because AVM may be the cause of seizures. ReferencesNguyen TN, Jovin TG, Nogueira RG, Zaidat OO, eds. Principles of neuroendovascular therapy. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 54. Patterson JT. Neurosurgery. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 68. Samaniego EA, Roa JA, Ortega-Gutierrez S, Derdeyn CP. Arteriovenous malformations and other vascular anomalies. In: Grotta JC, Albers GW, Broderick JP, et al, eds. Stroke: Pathophysiology, Diagnosis, and Management. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 30. | |
| |
Review Date: 10/23/2024 Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

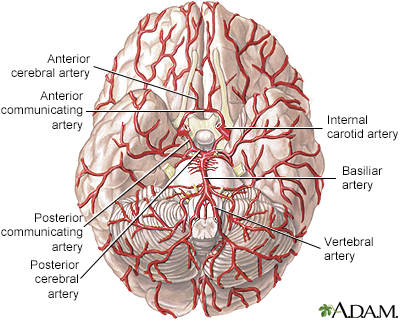 Arteries of the br...
Arteries of the br...
