Pregnancy SmartSiteTM
Water warts DefinitionMolluscum contagiosum is a viral skin infection that causes raised, pearl-like papules or nodules on the skin. CausesMolluscum contagiosum is caused by a virus that is a member of the poxvirus family. You can get the infection in different ways. This is a common infection in children and occurs when a child comes into direct contact with a skin lesion or an object that has the virus on it. (A skin lesion is an abnormal area of skin.) The infection is most often seen on the face, neck, armpit, arms, and hands. However, it can occur anywhere on the body, except it is rarely seen on the palms and soles. The virus can spread through contact with contaminated objects, such as towels, clothing, or toys. The virus also spreads by sexual contact. Early lesions on the genitals may be mistaken for herpes or warts. Unlike herpes, these lesions are painless. People with a weakened immune system (due to conditions such as HIV/AIDS) or severe eczema may have a rapidly spreading case of molluscum contagiosum. SymptomsThe infection on the skin begins as a small, painless papule, or bump. It may become raised to a pearly, flesh-colored nodule. The papule often has a dimple in the center. Scratching or other irritation causes the virus to spread in a line or in groups, called crops. The papules are about 0.08 to 0.20 inches (in) or 2 to 5 millimeters (mm) wide. Usually, there is no inflammation (swelling and redness) and no redness unless they have been irritated by rubbing or scratching. In adults, the lesions are commonly seen on the genitals, abdomen, and inner thigh. Exams and TestsYour health care provider will examine your skin and ask about your symptoms. Diagnosis is based on the appearance of the lesion. If needed, the diagnosis can be confirmed by removing one of the lesions to check for the virus under a microscope. TreatmentIn people with a healthy immune system, the disorder usually goes away on its own over months to years. But the lesions can spread before they go away. Although it's not necessary for a child to be treated, schools or daycare centers may ask parents to get their child treated to prevent spreading the infection to other children. Individual lesions may be removed with minor surgery. This is done by scraping, de-coring, freezing, or through needle electrosurgery. Laser treatment may also be used. Surgical removal of individual lesions may sometimes result in scarring. Medicines, such as salicylic acid preparations used to remove warts, may be helpful. Cantharidin is the most common solution used to treat the lesions in your provider's office. Tretinoin cream or imiquimod cream may also be prescribed. Outlook (Prognosis)Molluscum contagiosum lesions may persist from a few months to a few years. They eventually disappear without scarring, unless there has been excessive scratching, which may leave scars or discoloration. The disorder may persist in people with a weakened immune system. Possible ComplicationsProblems that can occur include any of the following:
When to Contact a Medical ProfessionalContact your provider if:
PreventionAvoid direct contact with the skin lesions of people who have molluscum contagiosum. Do not share towels or other personal items, such as razors and make-up, with other people. Male and female condoms can't fully protect you from getting molluscum contagiosum from a partner, as the virus can be on areas not covered by the condom. Even so, condoms should still be used every time the disease status of a sexual partner is unknown. Condoms reduce your chances of getting or spreading molluscum contagiosum and other STDs. ReferencesJames WD. Viral diseases. In: James WD, ed. Andrews' Diseases of the Skin: Clinical Dermatology. 14th ed. Philadelphia, PA: Elsevier; 2026:chap 14. Patterson JW. Viral diseases. In: Patterson JW, ed. Weedon's Skin Pathology. 6th ed. Philadelphia, PA: Elsevier Limited; 2025:chap 27. Seña AC, Swygard H, Cohen MS. Approach to the patient with a sexually transmitted infection. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 264. | |
| |
Review Date: 4/1/2025 Reviewed By: Elika Hoss, MD, Assistant Professor of Dermatology, Mayo Clinic, Scottsdale, AZ. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

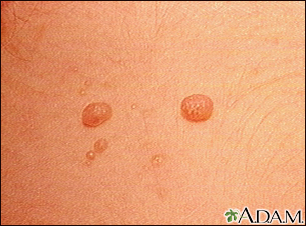 Molluscum contagio...
Molluscum contagio... Molluscum contagio...
Molluscum contagio... Molluscum on the c...
Molluscum on the c... Molluscum - micros...
Molluscum - micros... Molluscum contagio...
Molluscum contagio...
