Pregnancy SmartSiteTM
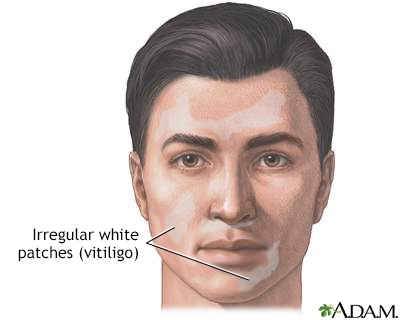
Autoimmune disorder - vitiligo DefinitionVitiligo is a skin condition in which there is a loss of color (pigment) from areas of skin. This results in uneven white patches that have no pigment, but the skin feels normal. CausesVitiligo occurs when immune cells destroy the cells that make brown pigment (melanocytes). This destruction is thought to be due to an autoimmune problem. An autoimmune disorder occurs when the body's immune system, which normally protects the body from infection, attacks and destroys healthy body tissue instead. The exact cause of vitiligo is unknown. Vitiligo may appear at any age. There is an increased rate of the condition in some families. Vitiligo is associated with other autoimmune diseases:
SymptomsFlat areas of normal-feeling skin without any pigment appear suddenly or gradually. These areas have a darker border. The edges are well defined, but irregular. Vitiligo most often affects the face, elbows and knees, back of the hands and feet, and genitals. It affects both sides of the body equally. Vitiligo is more noticeable in darker-skinned people because of the contrast of white patches against dark skin. No other skin changes occur. Exams and TestsYour health care provider can examine your skin to confirm the diagnosis. Sometimes, the provider uses a Wood lamp. This is a handheld ultraviolet light that causes the areas of skin with less pigment to glow bright white. In some cases, a skin biopsy may be needed to check for other causes of pigment loss. Your provider may also perform blood tests to check the levels of thyroid or other hormones, glucose level, and vitamin B12 to check for other associated disorders. TreatmentVitiligo is difficult to treat. Early treatment options include the following:
Skin may be moved (grafted) from normally pigmented areas and placed onto areas where there is pigment loss. Several cover-up makeups or skin dyes can mask vitiligo. Ask your provider for the names of these products. In extreme cases when most of the body is affected, the remaining skin that still has pigment may be depigmented, or bleached. This is a permanent change that is used as a last option. It is important to remember that skin without pigment is at greater risk for sun damage. Be sure to apply a broad-spectrum (UVA and UVB), high-SPF sunscreen or sunblock. Sunscreen can also be helpful for making the condition less noticeable, because unaffected skin may not darken in the sun. Use other safeguards against sun exposure, such as wearing a hat with a broad rim and long sleeve shirt and pants. Support GroupsMore information and support for people with vitiligo condition and their families can be found at:
Outlook (Prognosis)The course of vitiligo varies and is unpredictable. Some areas may regain normal pigment (coloring), but other new areas of pigment loss may appear. Skin that is repigmented may be slightly lighter or darker than the surrounding skin. Pigment loss may get worse over time. When to Contact a Medical ProfessionalContact your provider for an appointment if areas of your skin lose their coloring for no reason (for example, there was no injury to the skin). ReferencesDinulos JGH. Light-related diseases and disorders of pigmentation. In: Dinulos JGH, ed. Habif's Clinical Dermatology. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 19. Patterson JW. Disorders of pigmentation. In: Patterson JW, ed. Weedon's Skin Pathology. 5th ed. Philadelphia, PA: Elsevier; 2021:chap 11. Seneschal J, Passeron T, Torrelo A, Ortonne J-P. Vitiligo and other disorders of hypopigmentation. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 5th ed. Philadelphia, PA: Elsevier; 2025:chap 66. | |
| |
Review Date: 5/28/2024 Reviewed By: Ramin Fathi, MD, FAAD, Director, Phoenix Surgical Dermatology Group, Phoenix, AZ. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Vitiligo
Vitiligo Vitiligo - drug in...
Vitiligo - drug in... Vitiligo on the fa...
Vitiligo on the fa... Vitiligo on the ba...
Vitiligo on the ba...
