Pregnancy SmartSiteTM
Fungal infection - groin; Infection - fungal - groin; Ringworm - groin; Tinea cruris; Tinea of the groin DefinitionJock itch is an infection of the groin area caused by a fungus. The medical term is tinea cruris or ringworm of the groin. CausesJock itch occurs when a type of fungus grows and spreads in the groin area. Jock itch occurs mostly in adult men and teenage boys. Some people who have this infection also have athlete's foot or another kind of ringworm. The fungus that causes jock itch thrives in warm, moist areas. Jock itch can be triggered by friction from clothes and prolonged moistness in the groin area, such as from sweating. A fungal infection of the feet can spread to the groin area by pulling up pants if the waistband gets contaminated with fungus from the feet. Jock itch can be passed from one person to another by direct skin-to-skin contact or contact with unwashed clothing. SymptomsJock itch usually stays around the creases of the upper thigh and does not involve the scrotum or penis. Jock itch may spread to near the anus, causing anal itching and discomfort. Symptoms include:
Exams and TestsYour health care provider can usually diagnose jock itch based on how your skin looks. Tests are usually not necessary. If tests are needed, they may include:
TreatmentJock itch usually responds to self-care within a couple of weeks:
You may need treatment by your provider if your infection lasts longer than 2 weeks, is severe, or frequently returns. Your provider may prescribe:
If you tend to get jock itch, continue to apply antifungal medicine after bathing, even when you do not have jock itch. Jock itch is more common in overweight people with deep, moist skin folds. Losing weight may help prevent the condition from coming back. Outlook (Prognosis)Jock itch usually responds promptly to treatment. It is often less severe than other tinea infections, such as athlete's foot, but may last a long time. When to Contact a Medical ProfessionalContact your provider if jock itch does not respond to home care after 2 weeks or you have other symptoms. ReferencesElewski BE, Hughey LC, Hunt KM, Hay RJ. Fungal diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 5th ed. Philadelphia, PA: Elsevier; 2025:chap 77. Hay RJ. Dermatophytosis (ringworm) and other superficial mycoses. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 266. | |
| |
Review Date: 4/1/2025 Reviewed By: Elika Hoss, MD, Assistant Professor of Dermatology, Mayo Clinic, Scottsdale, AZ. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

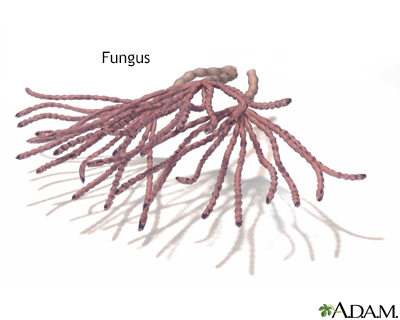 Fungus
Fungus
