Pregnancy SmartSiteTM
Tinea corporis; Fungal infection - body; Tinea circinata; Ringworm - body DefinitionRingworm is a skin infection that is caused by fungi. It is also called tinea. Related skin fungus infections may appear:
CausesFungi are germs that can live on the dead tissue of the hair, nails, and outer skin layers. Ringworm of the body is caused by mold-like fungi called dermatophytes. Ringworm of the body is common in children, but can occur in people of all ages. Fungi thrive in warm, moist areas. A ringworm infection is more likely if you:
Ringworm can spread quickly. You can catch it if you come into direct contact with an area of ringworm on someone's body. You can also get it by touching items that have the fungi on them, such as:
Pets can also spread ringworm. Cats are common carriers. SymptomsThe rash begins as a small area of red, raised spots and pimples. The rash slowly becomes ring-shaped, with a red, raised border and a clear center. The border may look scaly. The rash may occur on the arms, legs, face, or other exposed body areas. The area may be itchy. Exams and TestsYour health care provider can often diagnose ringworm by looking at your skin. You may also need the following tests:
TreatmentKeep your skin clean and dry. Use creams that treat fungal infections.
To use this medicine:
Your provider may prescribe medicine to take by mouth if your infection is very bad. A child with ringworm can return to school once treatment has started. To prevent the infection from spreading:
Infected pets should also be treated. This is because ringworm can spread from animals to humans by contact. Outlook (Prognosis)Ringworm often goes away within 4 weeks when using antifungal creams. The infection may spread to the feet, scalp, groin, or nails. Possible ComplicationsTwo complications of ringworm are:
When to Contact a Medical ProfessionalContact your provider if ringworm does not get better with self-care. ReferencesDinulos JGH. Superficial fungal infections. In: Dinulos JGH, ed. Habif's Clinical Dermatology. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 13. Elewski BE, Hughey LC, Hunt KM, Hay RJ. Fungal diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 5th ed. Philadelphia, PA: Elsevier; 2025:chap 77. Hay RJ. Dermatophytosis (ringworm) and other superficial mycoses. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 266. Patterson JW. Mycoses and algal infections. In: Patterson JW, ed. Weedon's Skin Pathology. 5th ed. Philadelphia, PA: Elsevier Limited; 2021:chap 26. | |
| |
Review Date: 10/13/2024 Reviewed By: Ramin Fathi, MD, FAAD, Director, Phoenix Surgical Dermatology Group, Phoenix, AZ. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Dermatitis - react...
Dermatitis - react... Ringworm - tinea c...
Ringworm - tinea c... Tinea versicolor -...
Tinea versicolor -... Tinea versicolor -...
Tinea versicolor -... Ringworm - tinea o...
Ringworm - tinea o...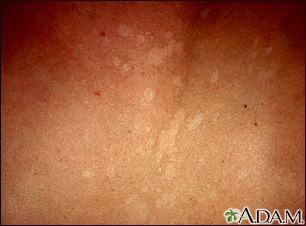 Tinea versicolor -...
Tinea versicolor -... Tinea versicolor o...
Tinea versicolor o... Ringworm - tinea m...
Ringworm - tinea m... Ringworm - tinea c...
Ringworm - tinea c... Granuloma - fungal...
Granuloma - fungal... Granuloma - fungal...
Granuloma - fungal... Tinea corporis - e...
Tinea corporis - e...
