Pregnancy SmartSiteTM
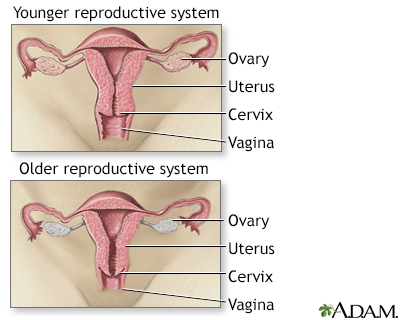
Perimenopause; Postmenopause DefinitionMenopause is the time in a woman's life when her periods (menstruation) stop. Most often, it is a natural, normal body change that occurs between ages 45 to 55. After menopause, a woman can no longer become pregnant. CausesDuring menopause, a woman's ovaries stop releasing eggs. Her body produces less of the female hormones estrogen and progesterone. Lower levels of these hormones cause menopause symptoms. Periods occur less often and eventually stop. Sometimes this happens suddenly. But most of the time, periods slowly stop over time. Menopause is complete when you have not had a period for 1 year. This is called postmenopause. Surgical menopause takes place when surgical treatments cause a drop in estrogen. This can happen if both of your ovaries are removed. Menopause can also sometimes be caused by drugs used for chemotherapy or hormone therapy (HT) for breast cancer. SymptomsSymptoms vary from woman to woman. They may last 5 or more years. Symptoms may be worse for some women than others. Symptoms of surgical menopause can be more severe and start more suddenly. The first thing you may notice is that periods start to change. They might occur more often or less often. Some women might get their period every 3 weeks before starting to skip periods You may have irregular periods for 1 to 3 years before they stop completely. 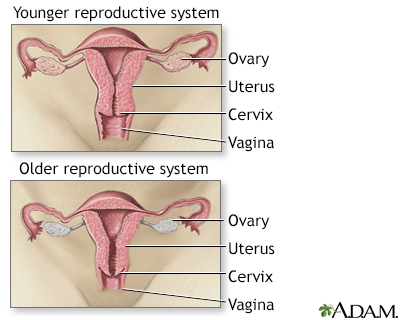 Common symptoms of menopause include:
Other symptoms of menopause may include:
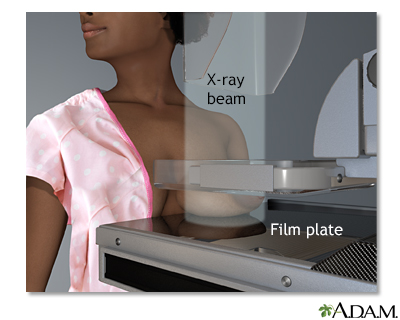
Exams and TestsBlood and urine tests can be used to look for changes in hormone levels. Test results can help your health care provider determine if you are close to menopause or if you have already gone through menopause. Your provider may need to repeat testing your hormone levels several times to confirm your menopausal status if you have not completely stopped menstruating. Tests that may be done include: Your provider will perform a pelvic exam. Decreased estrogen can cause changes in the lining of the vagina. Bone loss increases during the first few years after your last period. Your provider may order a bone density test to look for bone loss related to osteoporosis. This bone density test is recommended for all women at age 65 if they have not already had it. This test may be recommended sooner if you are at higher risk for osteoporosis because of your family history or medicines that you take. TreatmentTreatment may include lifestyle changes, HT, or both. Treatment depends on many factors such as:
HORMONE THERAPY HT may help if you have severe hot flashes, night sweats, mood issues, or vaginal dryness. HT is treatment with estrogen and, sometimes, progesterone. Talk to your provider about the benefits and risks of HT. Your provider should be aware of your entire medical and family history before prescribing HT. Several major studies have questioned the health benefits and risks of HT, including the risk of developing breast cancer, heart attacks, strokes, and blood clots. However, using HT for the 10 years after developing menopause is associated with a lower chance of death. Current guidelines support the use of HT for the treatment of hot flashes. Specific recommendations are:
To reduce the risks of estrogen therapy, your provider may recommend:
 Women who still have a uterus (that is, have not had surgery to remove it for any reason) should take estrogen combined with progesterone to prevent cancer of the lining of the uterus (endometrial cancer). ALTERNATIVES TO HORMONE THERAPY There are other medicines that can help with mood swings, hot flashes, and other symptoms. These include:
DIET AND LIFESTYLE CHANGES Lifestyle steps you can take to reduce menopause symptoms include: Diet changes:
Exercise and relaxation techniques:
Other tips:
Possible ComplicationsSome women have vaginal bleeding after menopause. This is often nothing to worry about. However, you should tell your provider if this happens, especially if it occurs more than a year after menopause. It may be an early sign of problems such as cancer. Your provider may do a biopsy of the uterine lining, a vaginal ultrasound, or both. Decreased estrogen level has been linked to some long-term effects, including:
When to Contact a Medical ProfessionalContact your provider if:
PreventionMenopause is a natural part of a woman's life. It does not need to be prevented. You can reduce your risk for long-term problems such as osteoporosis and heart disease by taking the following steps:
ReferencesAmerican College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 141: management of menopausal symptoms. Obstet Gynecol. 2014;123(1):202-216. PMID: 24463691 pubmed.ncbi.nlm.nih.gov/24463691/. Lobo RA. Menopause and care of the mature woman: endocrinology, consequences of estrogen deficiency, effects of hormone therapy, and other treatment options. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 14. North American Menopause Society Advisory Panel. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause. 2022;29(7):767-794. PMID: 35797481 pubmed.ncbi.nlm.nih.gov/28650869/. Rushing J, Skaznik-Wikiel ME, Santoro N. Menopause and perimenopause. In: Robertson RP ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 122. US Preventive Services Task Force, Grossman DC, Curry SJ, et al, eds. Vitamin D, calcium, or combined supplementation for the primary prevention of fractures in community-dwelling adults: US Preventive Services Task Force recommendation statement. JAMA. 2018;319(15):1592-1599. PMID: 29677309 pubmed.ncbi.nlm.nih.gov/29677309/. Van den Beld AW, Lamberts SWJ. Endocrinology and aging. In: Melmed S, Auchus, RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 28. | |
| |
Review Date: 7/12/2023 Reviewed By: John D. Jacobson, MD, Professor Emeritus, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Menopause
Menopause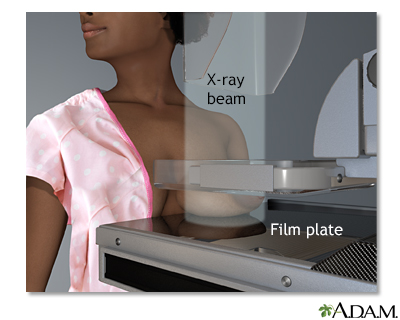 Mammogram
Mammogram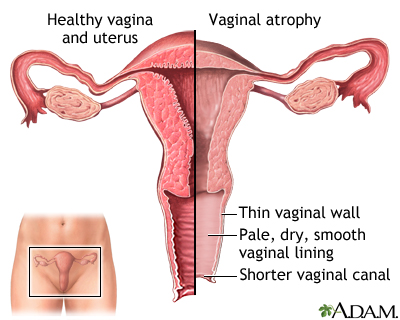 Vaginal atrophy
Vaginal atrophy
