Pregnancy SmartSiteTM
Threatened miscarriage; Threatened spontaneous abortion; Abortion - threatened; Threatened abortion; Early pregnancy loss; Spontaneous abortion DefinitionA threatened miscarriage is a condition that indicates the potential for a miscarriage or early pregnancy loss. It might take place before the 20th week of pregnancy. CausesSome pregnant women have some vaginal bleeding during the first 3 months of pregnancy. Bleeding may occur with or without abdominal cramps. When the symptoms indicate a miscarriage is possible, the condition is called a "threatened abortion." (This refers to a natural event that is not due to a medical or surgical abortion.) Miscarriage is common. Small falls, injuries or stress during the first trimester of pregnancy can cause threatened miscarriage. It occurs in almost one half of all pregnancies. The chance of miscarriage is higher in older women. About one half of women who have bleeding in the first trimester will have a miscarriage. SymptomsSymptoms of a threatened miscarriage include:
Note: During a miscarriage, low back pain or abdominal pain (dull to sharp, constant to intermittent) can occur. Tissue or clot-like material may pass from the vagina. Exams and TestsYour provider may perform an abdominal or vaginal ultrasound to check the baby's development and heartbeat, and the amount of bleeding. A pelvic exam may also be done to check your cervix. Blood tests done may include:
TreatmentApart from controlling the blood loss, you may not need any particular treatment. If you are Rh Negative, then you may be given immune globulin. You may be told to avoid or restrict some activities. Not having sexual intercourse is often recommended until the warning signs have disappeared. Outlook (Prognosis)Most women with a threatened miscarriage go on to have a normal pregnancy. Women who have had two or more miscarriages in a row may be more likely than other women to miscarry again. Possible ComplicationsComplications may include:
When to Contact a Medical ProfessionalIf you know you are (or are likely to be) pregnant and you have any symptoms of threatened miscarriage, contact your prenatal provider right away. PreventionMost miscarriages cannot be prevented. The most common cause of a miscarriage is a random genetic abnormality in the developing fetus. If you have two or more repeated miscarriages, you should consult a specialist to look for an underlying condition that is causing the problem. Women who get prenatal care have better pregnancy outcomes for themselves and their babies. A healthy pregnancy is more likely when you avoid things that are harmful to your pregnancy, such as:
Taking a prenatal vitamin or folic acid supplement before becoming pregnant and throughout your pregnancy can lower your chance of miscarriage and improve the chance of delivering a healthy baby. It is better to treat health problems before you get pregnant than to wait until you are already pregnant. Miscarriages caused by diseases that affect your whole body, such as high blood pressure, are rare. But you can prevent these miscarriages by detecting and treating the disease before becoming pregnant. Other factors that can increase your risk for miscarriage include:
ReferencesHenn MC, Lall MD. Complications of pregnancy. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 173. Richards DS. Obstetric ultrasound: imaging, dating, growth, and anomaly. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 9. Turocy J, Williams Z. Early and recurrent pregnancy loss: etiology, diagnosis, treatment. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 16. | |
| |
Review Date: 10/15/2024 Reviewed By: John D. Jacobson, MD, Professor Emeritus, Department of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

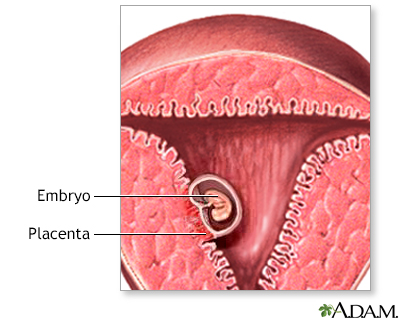 Early pregnancy
Early pregnancy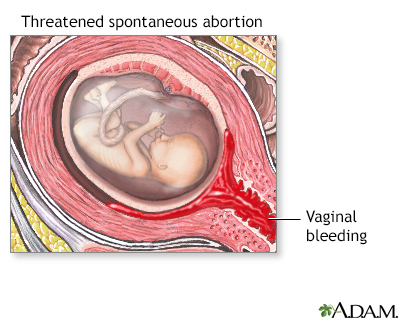 Threatened miscarr...
Threatened miscarr...
