Pregnancy SmartSiteTM
DefinitionOrbital cellulitis is an infection of the fat and muscles around the eye. It affects the eyelids, eyebrows, and cheeks. It may begin suddenly or be a result of an infection that gradually becomes worse. CausesOrbital cellulitis is a dangerous infection, which can cause lasting problems. Orbital cellulitis is different than periorbital cellulitis, which is an infection of the eyelid or skin around the eye. In children, it often starts out as a sinus infection from bacteria such as Haemophilus influenza. The infection used to be more common in young children, under the age of 7. It is now rare due to a vaccine that helps prevent this infection. The bacteria Staphylococcus aureus, Streptococcus pneumoniae, and beta-hemolytic streptococci may also cause orbital cellulitis. Orbital cellulitis infections in children may get worse very quickly and can lead to visual difficulties or blindness. Medical care is needed right away. SymptomsSymptoms may include:
Exams and TestsTests commonly done include:
Other tests may include:
TreatmentIn most cases, a hospital stay is needed. Treatment most often includes antibiotics given through a vein (IV). Surgery may be needed if there is an abscess or to relieve pressure in the space around the eye. In most cases, a hospital stay is needed. Treatment most often includes antibiotics given through a vein. Surgery may be needed to drain the or relieve pressure in the space around the eye. An orbital cellulitis infection can get worse very quickly. A person with this condition must be checked every few hours. Outlook (Prognosis)With prompt treatment, the person can recover fully. Possible ComplicationsComplications may include:
When to Contact a Medical ProfessionalOrbital cellulitis is a medical emergency that needs to be treated right away. Contact your health care provider if there are signs of eyelid swelling, especially with a fever. PreventionGetting scheduled HiB vaccine shots will prevent the infection in most children. Young children who share a household with a person who has this infection may need to take antibiotics to avoid getting sick. Prompt treatment of a sinus or dental infection may prevent it from spreading and becoming orbital cellulitis. ReferencesChi DH, Tobey A. Otolaryngology. In: Zitelli BJ, McIntire SC, Nowalk AJ, Garrison J, eds. Zitelli and Davis' Atlas of Pediatric Physical Diagnosis. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 24. Durand ML. Periocular infections. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 116. McNab AA. Orbital infection and inflammation. In: Yanoff M, Duker JS, eds. Ophthalmology. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 12.14. Olitsky SE, Marsh JD, Jackson MA. Orbital infections. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 674. | |
| |
Review Date: 8/29/2024 Reviewed By: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

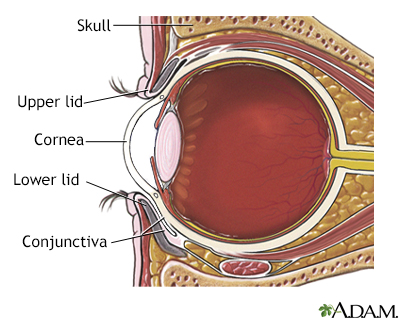 Eye anatomy
Eye anatomy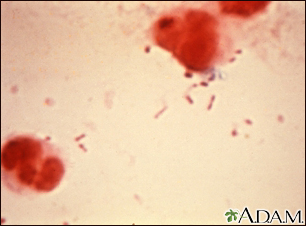 Haemophilus influe...
Haemophilus influe...
