Pregnancy SmartSiteTM
Vision changes - keratoconus DefinitionKeratoconus is an eye disease that affects the structure of the cornea. The cornea is the clear tissue that covers the front of the eye. With this condition, the shape of the cornea slowly changes from a round shape to a cone shape. It also gets thinner and the eye bulges out. This causes vision problems. In most people, these changes get worse over time. CausesThe cause is unknown. It is likely that the tendency to develop keratoconus is present from birth. The condition may be due to a defect in collagen. This is the tissue that provides the shape and strength to the cornea. Allergy and eye rubbing may speed up the damage. There is a link between keratoconus and Down syndrome. SymptomsThe earliest symptom is a slight blurring of vision that cannot be corrected with glasses. (Vision can most often be corrected to 20/20 with rigid, gas-permeable contact lenses.) Over time, you may see halos, have glare, or other night vision problems. Most people who develop keratoconus have a history of being nearsighted. The nearsightedness tends to become worse over time. As the problem gets worse, astigmatism develops and may worsen over time. Keratoconus is often discovered during the teenage years. It may also develop in older people. Exams and TestsThe most accurate test for this problem is called corneal topography, which creates a map of the curve of the cornea. A slit-lamp exam of the cornea can diagnose the disease in the later stages. A test called pachymetry can be used to measure the thickness of the cornea. TreatmentContact lenses are the main treatment for most patients with keratoconus. The lenses may provide good vision, but they do not treat or stop the condition. For many years, the only surgical treatment has been corneal transplantation. The following newer technologies may delay or prevent the need for corneal transplantation:
Outlook (Prognosis)In most cases, vision can be corrected with rigid gas-permeable contact lenses. If corneal transplantation is needed, results are very often good. However, the recovery period can be long. Many people still need contact lenses after the surgery. Possible ComplicationsIf left untreated, the cornea may thin to the point where a hole develops in the thinnest part. There is a risk of rejection after a cornea transplant, but the risk is much lower than with other organ transplants. You should not have laser vision correction (such as LASIK) if you have any degree of keratoconus. Corneal topography is done beforehand to rule out people with this condition. In rare cases, other laser vision correction procedures, such as PRK, may be safe for people with mild keratoconus. This may be more possible in people who have had corneal collagen cross-linking. When to Contact a Medical ProfessionalYoung people whose vision cannot be corrected to 20/20 with glasses should be checked by an eye doctor familiar with keratoconus. Parents with keratoconus should consider having their children screened for the disease starting at age 10. PreventionThere is no way to prevent this condition. Most health care providers believe that people should take steps to control allergies and avoid rubbing their eyes. ReferencesHernández-Quintela E, Sánchez-Huerta V, García-Albisua AM, Gulias-Cañizo R. Preoperative evaluation of keratoconus and ectasia. In: Azar DT, ed. Refractive Surgery. 3rd ed. Philadelphia, PA: Elsevier; 2020:chap 12. Sajjad A, Sugar J, Kang K. Keratoconus and other ectasias. In: Yanoff M, Duker JS, eds. Ophthalmology. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 4.18. | |
| |
Review Date: 7/9/2024 Reviewed By: Audrey Tai, DO, MS, Athena Eye Care, Mission Viejo, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

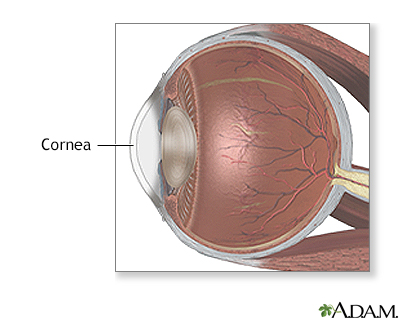 Cornea
Cornea
