Pregnancy SmartSiteTM
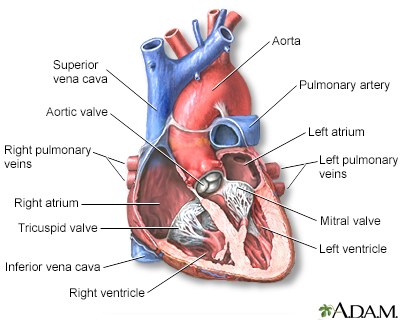
Right-to-left cardiac shunt; Right-to-left circulatory shunt DefinitionCyanotic heart disease refers to a group of many different heart defects that are present at birth (congenital). They result in a low blood oxygen level. Cyanosis refers to a bluish color of the skin and mucous membranes due to the low oxygen level. CausesNormally, blood returns from the body and flows through the heart and lungs.
Heart defects that children are born with can change the way blood flows through the heart and lungs. These defects can cause less blood to flow to the lungs. They can also result in blue and red blood mixing together. This causes poorly oxygenated blood to be pumped out to the body. As a result:
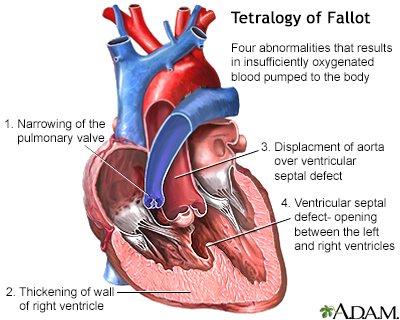
Some of these heart defects involve the heart valves. These defects force blue blood to mix with red blood through abnormal heart channels. Heart valves are found between the heart and the large blood vessels that bring blood to and from the heart. These valves open up enough for blood to flow through. Then they close, keeping blood from flowing backward. Heart valve defects that can cause cyanosis include:
Other heart defects may include abnormalities in valve development or in the location and connections between blood vessels. Some examples include:
 Certain medical conditions in the mother can increase the risk of certain cyanotic heart diseases in the infant. Some examples include:
SymptomsSome heart defects cause major problems right after birth. The main symptom of cyanosis is a bluish color of the lips, fingers, and toes that is caused by the low oxygen content in the blood. It may occur while the child is resting or only when the child is active. 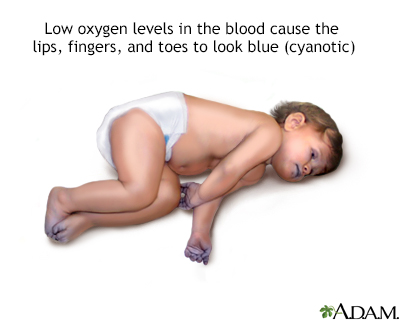 Some children have breathing problems (dyspnea). They may get into a squatting position after physical activity to relieve breathlessness. Others have spells, in which their bodies are suddenly starved of oxygen. During these spells, symptoms may include:
Infants may get tired or sweat while feeding and may not gain as much weight as they should. Fainting (syncope) and chest pain may occur. Other symptoms depend on the type of cyanotic heart disease, and may include:
Exams and TestsPhysical examination confirms cyanosis. Older children may have clubbed fingers. The provider will listen to the heart and lungs with a stethoscope. Abnormal heart sounds, a heart murmur, and lung crackles may be heard. Tests will vary depending on the cause, but may include:
TreatmentSome infants may need to stay in the hospital after birth so they can receive oxygen or be put on a breathing machine. They may receive medicines to:
The treatment of choice for most congenital heart diseases is surgery to repair the defect. There are many types of surgery, depending on the kind of birth defect. Surgery may be needed soon after birth, or it may be delayed for months or even years. Some surgeries may be staged as the child grows. Your child may need to take water pills (diuretics) and other heart medicines before or after surgery. Be sure to follow the correct dosage. Regular follow-up with the surgeon is important. Many children who have had heart surgery must take antibiotics before, and sometimes after having any dental work or other medical procedures. Make sure you have clear instructions from your child's heart doctor (cardiologist). Ask your child's provider before getting any immunizations. Most children can follow the recommended guidelines for childhood vaccinations. Outlook (Prognosis)The outlook depends on the specific disorder and its severity. Possible ComplicationsComplications of cyanotic heart disease include:
When to Contact a Medical ProfessionalContact your child's provider right away if your baby has:
PreventionSome inherited factors may play a role in congenital heart disease. Many family members may be affected. If you are planning to get pregnant, talk to your provider about screening for genetic diseases. Women who plan to become pregnant should be immunized against rubella if they are not already immune. Rubella infection in a pregnant woman can cause congenital heart disease. Women who are pregnant should get good prenatal care:
ReferencesBernstein D. Cyanotic congenital heart disease: evaluation of the critically ill neonate with cyanosis and respiratory distress. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 478. Valente AM, Dorfman AL, Babu-Narayan SV, Kreiger EV. Congenital heart disease in the adolescent and adult. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 82. Well A, Fraser CD. Congenital heart disease. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 59. | |
| |
Review Date: 10/1/2025 Reviewed By: Thomas S. Metkus MD, PhD, Associate Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Heart - section th...
Heart - section th...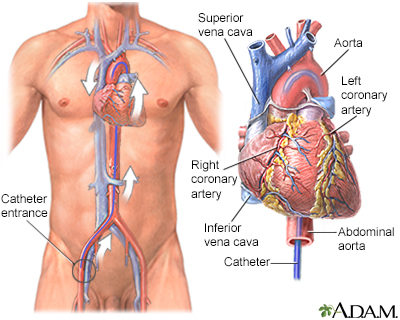 Cardiac catheteriz...
Cardiac catheteriz...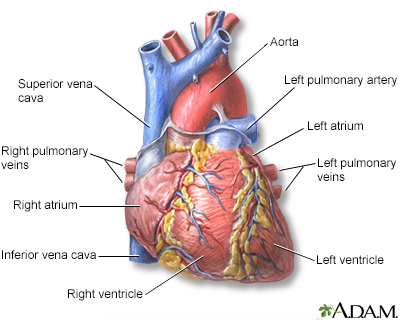 Heart - front view
Heart - front view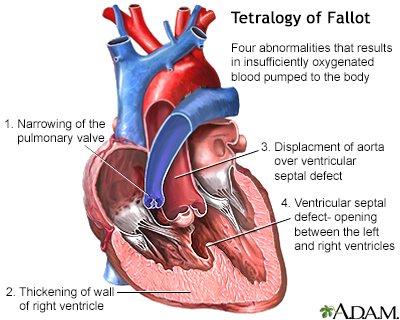 Tetralogy of Fallo
Tetralogy of Fallo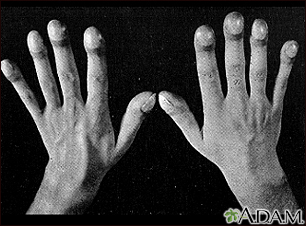 Clubbing
Clubbing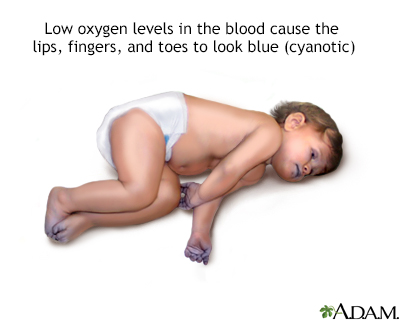 Cyanotic heart dis...
Cyanotic heart dis...
