Pregnancy SmartSiteTM
PAIS; Androgen insensitivity syndrome - partial; Incomplete testicular feminization; Type I familial incomplete male pseudohermaphroditism; Lubs syndrome; Reifenstein syndrome; Rosewater syndrome; Partial androgen insensitivity syndrome - Intersex; Differences of sex development DefinitionPartial androgen insensitivity syndrome (PAIS) is when a person who has one X and one Y chromosome (typically seen in males) but is resistant to hormones that produce a male appearance (called androgens). As a result, the person has some of the physical traits of a female, but the genetic makeup of a male. PAIS is a type of androgen insensitivity syndrome (AIS). AIS is one of the conditions that are described as differences of sex development (DSD). CausesIn the first 2 to 3 months of pregnancy, all babies have the same genitals. As a baby grows inside the womb, male or female genitals develop depending on the pair of sex chromosomes the baby has from the parents (XY for male, XX for female). It also depends on the levels of androgens. In a baby with XY chromosomes, high levels of androgens are made in the testes. This baby will develop male genitals. In a baby with XX chromosomes, there are no testes and the levels of androgens are very low. This baby will develop female genitals. PAIS is caused by genetic defects on the X chromosome. These defects make the body less able to respond to androgens. This leads to problems with the development of the male sex organs. At birth, the baby may have ambiguous external genitals. This means that they do not look typically either male or female. The syndrome is passed down genetically (X-linked recessive inheritance). People with two X chromosomes are not affected if only one copy of the X chromosome carries the genetic variant. Males who inherit the gene from their mothers will have the condition. There is a 50% chance that a male child of a mother with the genetic trait will be affected. Every female child of a mother with the genetic trait has a 50% chance of carrying the genetic trait. Family history is important in determining risk factors of PAIS. SymptomsPeople with PAIS may have both male and female physical characteristics. These characteristics vary from person to person. These may include:
Exams and TestsPAIS is often discovered during childhood because the person may have both male and female physical characteristics. The health care provider will perform a physical exam. Tests may include:
TreatmentInfants with PAIS may be assigned a gender depending on the extent of genital ambiguity. However, gender assignment is a complex issue, and the need for it and the timing of it must be considered carefully. PAIS can be distressing for parents and families. While early surgery may make the parents feel more comfortable, the child may not be happy with the decision as they become older. Many health experts and intersex advocates suggest waiting until the child is old enough to be involved in the decision, unless surgery is needed for the health of the infant. Possible treatments for PAIS include:
Treatment and gender assignment can be a very complex issue and must be targeted to each individual person. Treatment guidelines are still evolving. It is vital that children with PAIS and their parents receive care and support from a health care team that includes different specialists with expertise in gender medicine. This should include mental health professionals to help provide support for both children and their parents. Support GroupsThe following groups can provide more information on PAIS:
Outlook (Prognosis)Androgens are most important during early development in the womb. People with PAIS can have a normal lifespan and be totally healthy, but they may have difficulty conceiving a child. Possible ComplicationsPossible complications may include:
When to Contact a Medical ProfessionalContact your health care provider if your child has signs or symptoms of the syndrome. Genetic testing and counseling are recommended if PAIS is suspected. PreventionPrenatal testing is available. People with a family history of PAIS should consider genetic counseling. ReferencesChan Y-M, Hannema SE, Achermann JC, Hughes IA. Disorders of sex development. In: Melmed S, Auchus, RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 24. Délot EC, Vilain E. Differences of sex development. In: Strauss JF, Barbieri R, Dokras A, Williams CJ, Williams Z, eds. Yen & Jaffe's Reproductive Endocrinology. 9th ed. Elsevier; 2024:chap 17. Donohoue PA. Disorders of sex development. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 606. Genetic and Rare Diseases Information Center website. Partial androgen insensitivity syndrome. rarediseases.info.nih.gov/diseases/5692/partial-androgen-insensitivity-syndrome. Updated February 2024. Accessed March 20, 2024. Matsumoto AM, Anawalt BD. Testicular disorders. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 19. Shnorhavorian M, Fechner PY. Differences in sex development. In: Gleason CA, Sawyer T, eds. Avery's Diseases of the Newborn. 11th ed. Philadelphia, PA: Elsevier; 2024:chap 85. Yu RN, Diamond DA. Disorders of sexual development: etiology, evaluation, and medical management. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 48. | |
| |
Review Date: 3/12/2024 Reviewed By: Anna C. Edens Hurst, MD, MS, Associate Professor in Medical Genetics, The University of Alabama at Birmingham, Birmingham, AL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

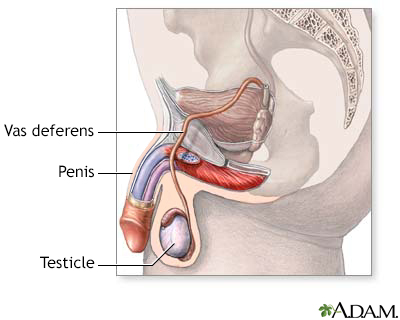 Male reproductive ...
Male reproductive ...
