Pregnancy SmartSiteTM
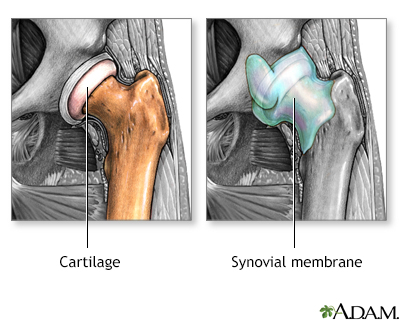
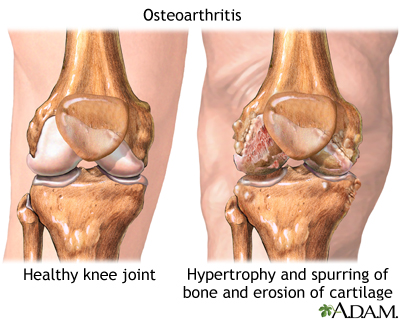
Joint inflammation; Joint degeneration DefinitionArthritis is inflammation or degeneration of one or more joints. A joint is the area where 2 bones meet. There are more than 100 different types of arthritis. CausesArthritis involves the breakdown of structures of the joint, particularly cartilage. Normal cartilage protects a joint and allows it to move smoothly. Cartilage also absorbs shock when pressure is placed on the joint, such as when you walk. Without the normal amount of cartilage, the bones under the cartilage become damaged and rub together. This causes swelling (inflammation), and stiffness. 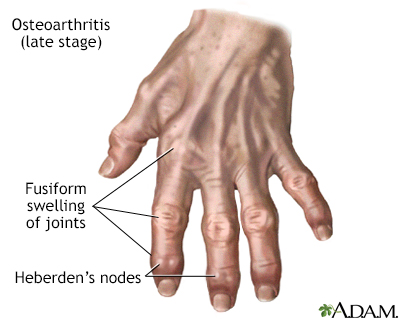 Other joint structures affected by arthritis include:
Joint inflammation and damage may result from:
In most cases, the joint inflammation goes away after the cause goes away or is treated. Sometimes, it does not. When this happens, you have long-term (chronic) arthritis. Arthritis may occur in people of any age and sex. Osteoarthritis, which is due to non-inflammatory processes and increases with age, is the most common type. Other, more common types of inflammatory arthritis include:
 SymptomsArthritis causes joint pain, swelling, stiffness, and limited movement. Symptoms can include:
Exams and TestsThe health care provider will perform a physical exam and ask about your medical history. The physical exam may show:
Some types of arthritis may cause joint deformity. This may be a sign of severe, untreated rheumatoid arthritis or of osteoarthritis. Blood tests and joint x-rays are often done to check for infection and other causes of arthritis. The provider may also remove a sample of joint fluid with a needle and send it to a lab to be checked for inflammation crystals or infection. TreatmentThe underlying cause often cannot be cured. The goal of treatment is to:
LIFESTYLE CHANGES Lifestyle changes are the preferred treatment for osteoarthritis and other types of joint swelling. Exercise can help relieve stiffness, reduce pain and fatigue, and improve muscle and bone strength. Your health care team can help you design an exercise program that is best for you. Exercise programs may include:
Your provider may suggest physical therapy. This might include:
Other things you can do include:
MEDICINES Medicines may be prescribed along with lifestyle changes. All medicines have some risks. You should be closely followed by a provider when taking arthritis medicines, even ones you buy over-the-counter. Over-the-counter medicines:
Depending on the type of arthritis, a number of other medicines may be prescribed:
It is very important to take your medicines as directed by your provider. If you are having problems doing so (for example, because of side effects), you should talk to your provider. Also make sure your provider knows about all the medicines you are taking, including vitamins and supplements bought without a prescription. SURGERY AND OTHER TREATMENTS In some cases, surgery may be done if other treatments have not worked and severe damage to a joint occurs. This may include:
Outlook (Prognosis)A few arthritis-related disorders can be completely cured with proper treatment. Yet, many of these disorders become long-term (chronic) health problems but can often be well-controlled. Aggressive forms of some arthritic conditions may have significant effects on mobility and may lead to involvement of other body organs or systems. Possible ComplicationsComplications of arthritis include:
When to Contact a Medical ProfessionalContact your provider if:
PreventionEarly diagnosis and treatment can help prevent joint damage. If you have a family history of arthritis, tell your provider, even if you do not have joint pain. Avoiding excessive, repeated motions may help protect you against osteoarthritis. ReferencesBykerk VP, Crow MK. Approach to the patient with rheumatic disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 236. Fraenkel L, Bathon JM, England BR, et al. 2021 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol. 2021;73(7):1108-1123. PMID: 34101376 pubmed.ncbi.nlm.nih.gov/34101376/. Hunter DJ. Osteoarthritis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 241. Inman RD, Rahman P. Spondyloarthritis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 244. McInnes IB. Rheumatoid arthritis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 243. | |
| |
Review Date: 12/31/2023 Reviewed By: Neil J. Gonter, MD, Assistant Professor of Medicine, Columbia University, NY and private practice specializing in Rheumatology at Rheumatology Associates of North Jersey, Teaneck, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Osteoarthritis
Osteoarthritis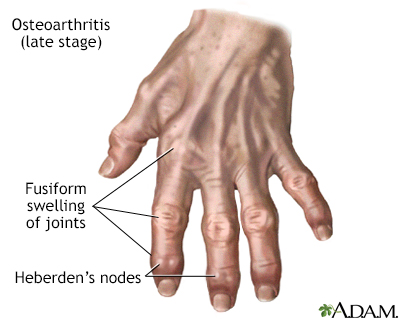 Osteoarthritis
Osteoarthritis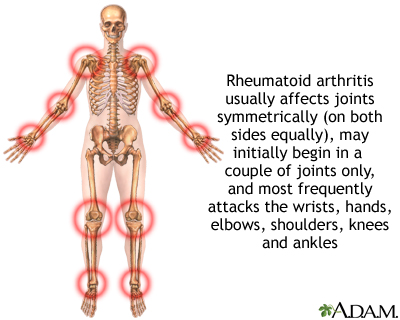 Rheumatoid arthrit...
Rheumatoid arthrit...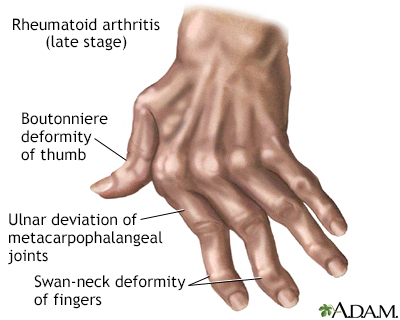 Rheumatoid arthrit...
Rheumatoid arthrit...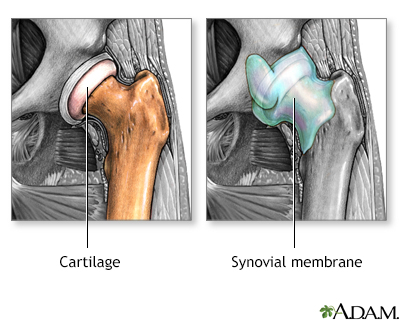 Osteoarthritis vs....
Osteoarthritis vs....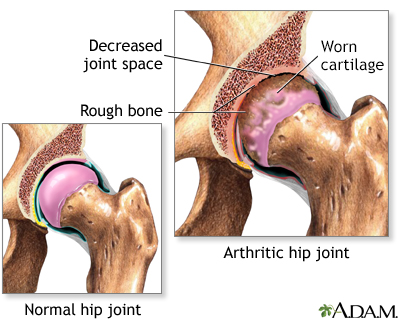 Arthritis in hip
Arthritis in hip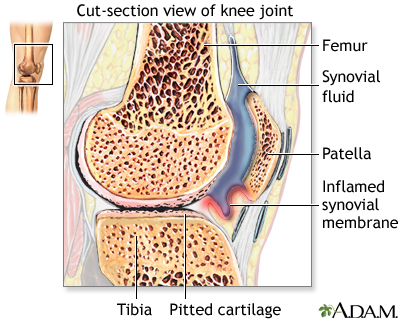 Rheumatoid arthrit...
Rheumatoid arthrit...
