Pregnancy SmartSiteTM
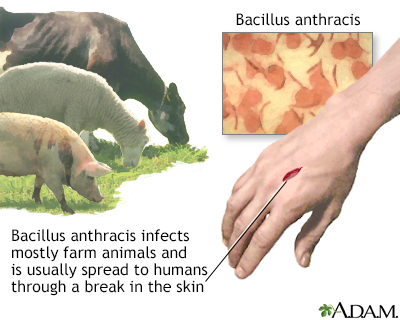
Woolsorter's disease; Ragpicker's disease; Cutaneous anthrax; Gastrointestinal anthrax DefinitionAnthrax is an infectious disease caused by a bacterium called Bacillus anthracis. Infection in humans most often involves the skin, gastrointestinal tract, or lungs. CausesAnthrax commonly affects hoofed animals such as sheep, cattle, and goats. Humans who come into contact with infected animals can get sick with anthrax as well. There are three main routes of anthrax infection: skin (cutaneous), lung (inhalation), and mouth (gastrointestinal). Cutaneous anthrax occurs when anthrax spores enter the body through a cut or scrape on the skin.
Inhalational anthrax develops when anthrax spores enter the lungs through the airways. It is most commonly contracted when workers breathe in airborne anthrax spores during processes such as tanning hides and processing wool. Breathing in spores means a person has been exposed to anthrax. But it does not mean the person will have symptoms.
Gastrointestinal anthrax occurs when someone eats anthrax-tainted meat. Injection anthrax can occur in someone who self-injects drugs (heroin). Anthrax may be used as a biological weapon or for bioterrorism. SymptomsSymptoms of anthrax differ, depending on the type of anthrax. Symptoms of cutaneous anthrax start 1 to 7 days after exposure:
Symptoms of inhalational anthrax:
Symptoms of gastrointestinal anthrax usually occur within 1 week and may include:
Symptoms of injection anthrax are similar to those of cutaneous anthrax. In addition, the skin or muscle beneath the injection site may get infected. Exams and TestsYour health care provider will perform a physical exam. The tests to diagnose anthrax depend on the type of disease that is suspected. A culture of the skin, and sometimes a biopsy, are done on the skin sores. The sample is looked at under a microscope to identify the anthrax bacterium. Tests may include:
More tests may be done on fluid or blood samples. TreatmentAntibiotics are usually used to treat anthrax. Antibiotics that may be prescribed include penicillin, doxycycline, and ciprofloxacin. Inhalational anthrax is treated with a combination of antibiotics such as ciprofloxacin plus another medicine. They are given by IV (intravenously). Antibiotics are usually taken for 60 days because it can take spores that long to germinate. Cutaneous anthrax is treated with antibiotics taken by mouth, usually for 7 to 10 days. Doxycycline and ciprofloxacin are most often used. Outlook (Prognosis)When treated with antibiotics, cutaneous anthrax is likely to get better. But some people who do not get treated may die if anthrax spreads to the blood. People with second-stage inhalational anthrax have a poor outlook, even with antibiotic therapy. Many cases in the second stage are fatal. Gastrointestinal anthrax infection can spread to the bloodstream and may result in death. When to Contact a Medical ProfessionalContact your provider if you think you have been exposed to anthrax or if you develop symptoms of any type of anthrax. PreventionThere are two main ways to prevent anthrax:
There is no known way to spread cutaneous anthrax from person to person. People who live with someone who has cutaneous anthrax do not need antibiotics unless they have also been exposed to the same source of anthrax. ReferencesCenters for Disease Control and Prevention website. Anthrax. About anthrax. www.cdc.gov/anthrax/about/index.html. Updated April 2, 2025. Accessed May 20. 2025. Kortepeter MG, Cieslak TJ. Bioterrorism. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 19. Martin GJ, Friedlander AM. Bacillus anthracis (anthrax). In: Blaser MJ, Cohen JI, Holland SM, et al, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 10th ed. Philadelphia, PA: Elsevier; 2026:chap 212. | |
| |
Review Date: 5/12/2025 Reviewed By: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Cutaneous anthrax
Cutaneous anthrax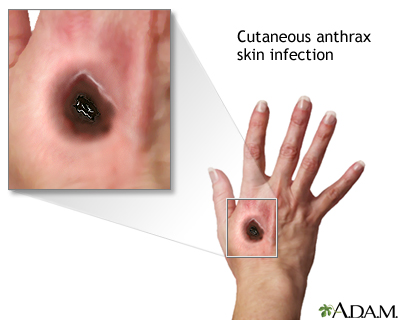 Cutaneous Anthrax
Cutaneous Anthrax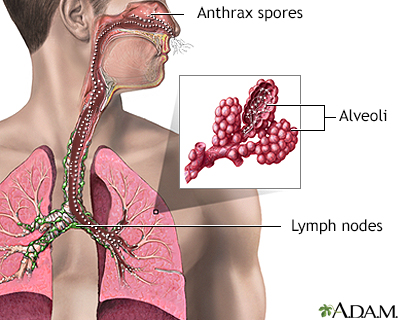 Inhalation Anthrax
Inhalation Anthrax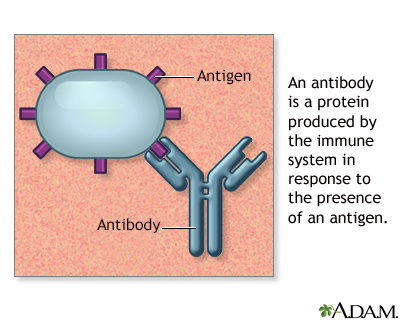 Antibodies
Antibodies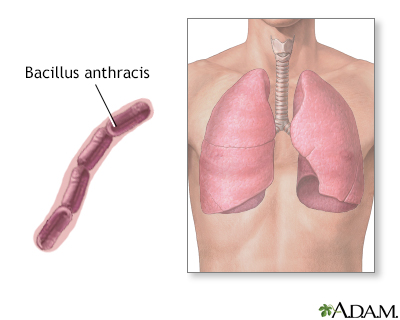 Bacillus anthracis
Bacillus anthracis
