Pregnancy SmartSiteTM
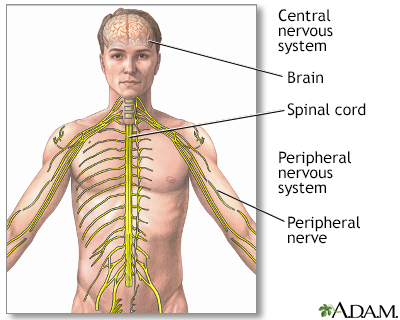
Nerve pain; Painful neuropathy; Neuropathic pain DefinitionNeuralgia is a sharp, shocking pain that follows the path of a nerve and is due to irritation or damage to the nerve. Common neuralgias include:
CausesCauses of neuralgia include:
In many cases, the cause is unknown. Postherpetic neuralgia and trigeminal neuralgia are the two most common forms of neuralgia. A related but less common neuralgia affects the glossopharyngeal nerve, which provides feeling to the throat. Neuralgia is more common in older people, but it may occur at any age. SymptomsSymptoms may include any of the following:
Exams and TestsYour health care provider will perform a physical exam, and ask about your symptoms. The exam may show:
You may also need to see a dentist if the pain is in your face or jaw. A dental exam can check for dental disorders that may cause facial pain (such as a tooth abscess). Other symptoms (such as redness or swelling) may indicate other conditions such as infections, bone fractures, or rheumatoid arthritis. There are no specific tests for neuralgia. But, the following tests may be done to find the cause of the pain:
TreatmentTreatment depends on the cause, location, and severity of the pain. Medicines to control pain may include:
Other treatments may include:
Procedures may not improve symptoms and can cause loss of feeling or abnormal sensations. When other treatments fail, providers may try nerve or spinal cord stimulation. In rare cases, a procedure called motor cortex stimulation (MCS) is tried. An electrode is placed over part of a nerve, spinal cord, or brain and is hooked to a pulse generator under the skin. This changes how your nerves signal and it may reduce pain. Outlook (Prognosis)Most neuralgias are not life threatening and are not signs of other life-threatening disorders. For severe pain that does not improve, see a pain specialist so that you can explore all treatment options. Most neuralgias respond to treatment. Attacks of pain usually come and go. But, attacks may become more frequent in some people as they get older. Sometimes, the condition may improve on its own or disappear with time, even when the cause is not found. Possible ComplicationsComplications may include:
When to Contact a Medical ProfessionalContact your provider if:
PreventionStrict control of blood sugar may prevent nerve damage in people with diabetes. In the case of shingles, antiviral medicines and the herpes zoster virus vaccine may prevent neuralgia. ReferencesCohen SP. Pain. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 388. Katirji B. Disorders of peripheral nerves. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 106. Smith AG, Shy ME. Peripheral neuropathies. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 388. | |
| |
Review Date: 6/13/2024 Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Central nervous sy...
Central nervous sy...
