Contraception; Family planning and contraception; Coitus interruptus
Definition
Your choice of a birth control method depends on a number of factors, including your health, how often you have sexual intercourse, and whether or not you want children.
Information
Here are some questions to consider when selecting a birth control method:
- How well does the method prevent pregnancy? To tell how well a method works, look at the number of pregnancies in 100 women using that method over a period of 1 year.
- What are your feelings about getting pregnant? Would an unplanned pregnancy create hardship or distress to a woman or her partner? Or would a pregnancy be welcomed if it occurred earlier than planned?
- How much does a method of birth control cost? Does your insurance plan pay for it?
- What are the health risks? Talk about these risks with your health care provider before believing what you hear from others.
- Is your partner willing to accept and use a given method of birth control?
- Do you want a method that you only need to use when you have sex? Or do you want something that is in place and always working?
- Is preventing infections spread by sexual contact important? Many methods do not protect you from sexually transmitted infections (STIs). Condoms are the best choice for preventing STIs. They work best when combined with spermicides.
- Availability: Can the method be used without a prescription, a provider visit, or, in the case of minors, parental consent?
BARRIER METHODS OF BIRTH CONTROL
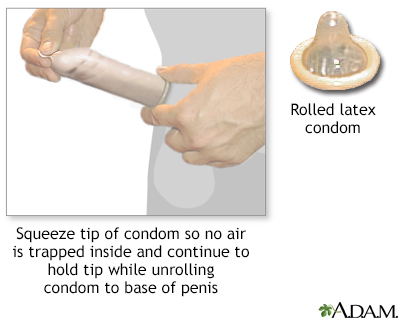
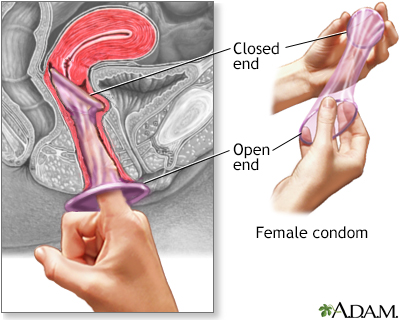
CONDOMS:
- A condom is a thin latex or polyurethane sheath. The male condom is placed around the erect penis. The female condom is placed inside the vagina before intercourse.
- A condom must be worn at all times during intercourse to prevent pregnancy.
- Condoms can be bought in most drug and grocery stores. Some family planning clinics offer free condoms. You do not need a prescription to get condoms.
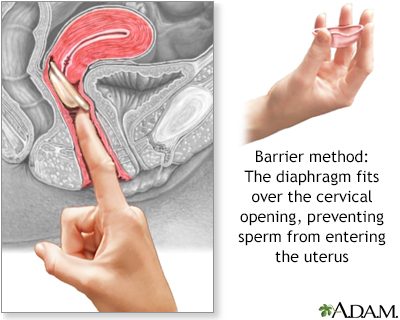
DIAPHRAGM AND CERVICAL CAP:
- A diaphragm is a flexible rubber cup that is filled with spermicidal cream or jelly.
- It is placed into the vagina over the cervix before intercourse, to prevent sperm from reaching the uterus.
- It should be left in place for 6 to 8 hours after intercourse.
- Diaphragms must be prescribed by a woman's provider. The provider will determine the correct type and size of diaphragm for the woman.
- About 5 to 20 pregnancies occur over 1 year in 100 women using this method, depending on proper use.
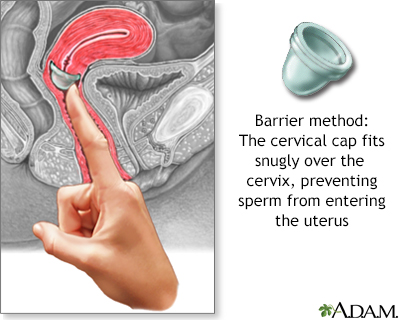
- A similar, smaller device is called a cervical cap.
- Risks include irritation and allergic reactions to the diaphragm or spermicide, and increased frequency of urinary tract infection and vaginal yeast infection. In rare cases, toxic shock syndrome may develop in women who leave the diaphragm in too long. A cervical cap may cause an abnormal Pap test.
VAGINAL SPONGE:
- Vaginal contraceptive sponges are soft, and contain a chemical that kills or "disables" sperm.
- The sponge is moistened and inserted into the vagina, to cover over the cervix before intercourse.
- The vaginal sponge can be bought at your pharmacy without a prescription.
HORMONAL METHODS OF BIRTH CONTROL
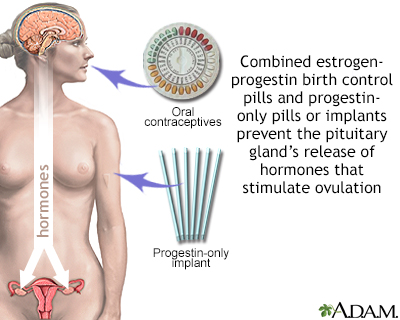
Some birth control methods use hormones. They will have either both an estrogen and a progestin, or a progestin alone. You need a prescription for most hormonal birth control methods.
- Both hormones prevent a woman's ovary from releasing an egg during her cycle. They do this by affecting the levels of other hormones the body makes.
- Progestins help prevent sperm from making their way to the egg by making mucus around a woman's cervix thick and sticky.
Types of hormonal birth control methods include:
- Birth control pills: These may contain both estrogen and progestin, or only progestin.
- Implants: These are small rods implanted beneath the skin. They release a continuous dose of hormone to prevent ovulation.
- Progestin injections, such as Depo-Provera, that are given into the muscles of the upper arm or buttocks once every 3 months.
- The skin patch, such as Ortho Evra, is placed on your shoulder, buttocks, or other place on the body. It releases a continuous dose of hormones.
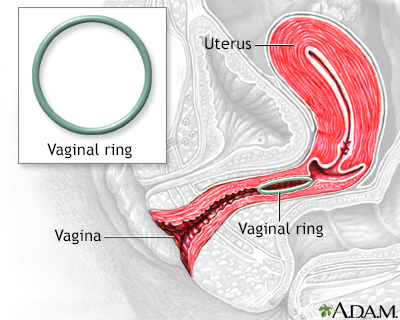
- The vaginal ring, such as NuvaRing, is a flexible ring about 2 inches (5 centimeters) wide. It is placed into the vagina. It releases the hormones progestin and estrogen.
- Emergency (or "morning after") contraception: This medicine can be bought without a prescription at your drugstore.
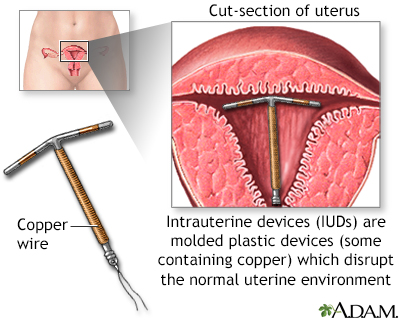
IUD (INTRAUTERINE DEVICE):
- The IUD is a small plastic or copper device placed inside the woman's uterus by her provider. Some IUDs release small amounts of progestin. IUDs may be left in place for 3 to 10 years, depending on the device used.
- IUDs can be placed at almost any time.
- IUDs are safe and work well. Fewer than 1 out of 100 women per year will get pregnant using an IUD.
- IUDs that release progestin may be for treating heavy menstrual bleeding and reducing cramps. They may also cause periods to stop completely.
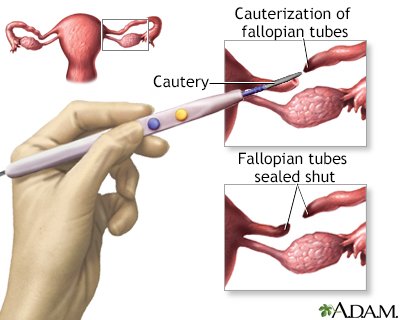
PERMANENT METHODS OF BIRTH CONTROL
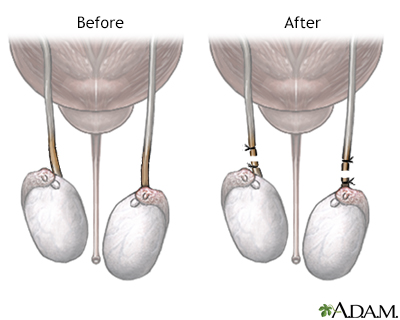
These methods are best for men, women, and couples who feel certain they do not want to have children in the future. They include vasectomy and tubal ligation. These procedures can sometimes be reversed if a pregnancy is desired at a later time. However, the success rate for reversal is not high.
BIRTH CONTROL METHODS THAT DO NOT WORK VERY WELL
- Withdrawal of the penis from the vagina before ejaculation can still result in pregnancy. Some semen often escapes before full withdrawal. It can be enough to cause a pregnancy.
- Douching shortly after sex is not likely to work. The sperm can make their way past the cervix within 90 seconds. Douching is never recommended because it can cause infections in the uterus and tubes.
- Breastfeeding: Despite the myths, women who are breastfeeding can become pregnant.
References
American College of Obstetricians and Gynecologists website. ACOG Practice Bulletin No. 206: Use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2019;133(6):1288. Erratum for: Obstet Gynecol. 2019;133(2):e128-e150. PMID: 31135757 pubmed.ncbi.nlm.nih.gov/31135757/.
Committee on Adolescent Health Care. Committee Opinion No 699: Adolescent pregnancy, contraception, and sexual activity. Obstet Gynecol. 2017;129(5):e142-e149. PMID: 28426620 pubmed.ncbi.nlm.nih.gov/28426620/.
Curtis KM, Jatlaoui TC, Tepper NK, et al. US selected practice recommendations for contraceptive use, 2016. MMWR Recomm Rep. 2016;65(4):1-66. PMID: 27467319 pubmed.ncbi.nlm.nih.gov/27467319/.
Harper DM, Wilfling LE, Blanner CF. Contraception. In: Rakel RE, Rakel DP, eds. Textbook of Family Medicine. 9th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 26.
Romano ME, Alderman EM. Contraception. In: Kliegman RM, St. Geme JW, Blum NJ, eds, et al. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 160.
Rivlin K, Davis AR. Contraception and abortion. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 13.

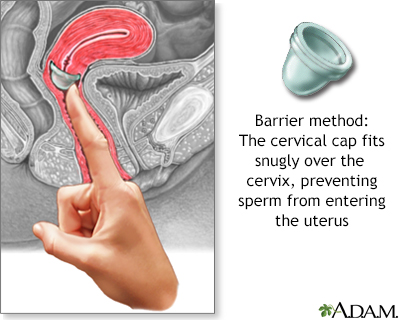 The cervical cap
The cervical cap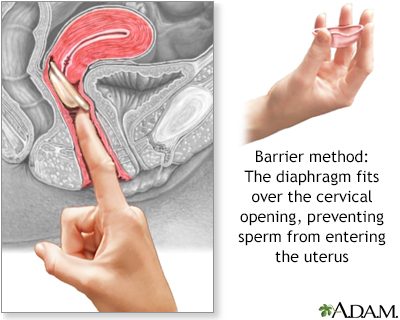 The diaphragm
The diaphragm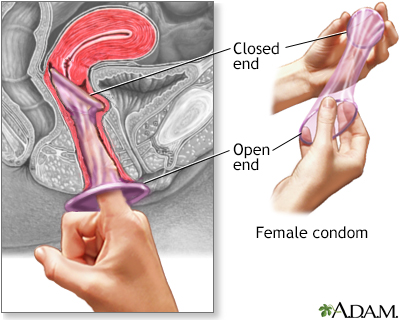 The female condom
The female condom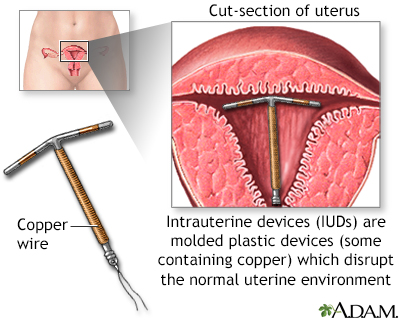 Intrauterine devic
Intrauterine devic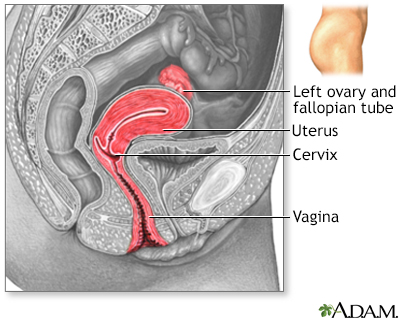 Side sectional vie...
Side sectional vie...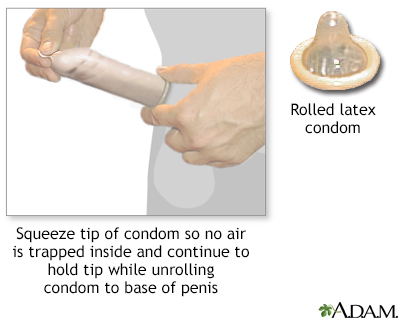 The male condom
The male condom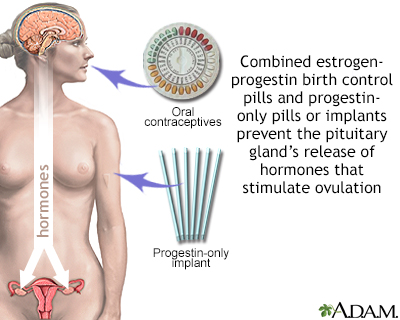 Hormone-based cont...
Hormone-based cont...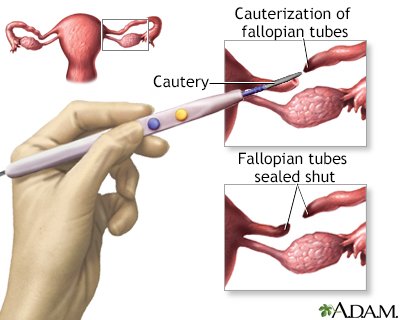 Tubal ligation
Tubal ligation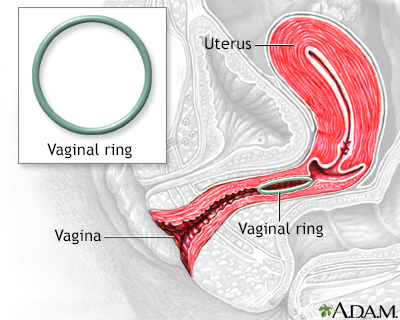 Vaginal ring
Vaginal ring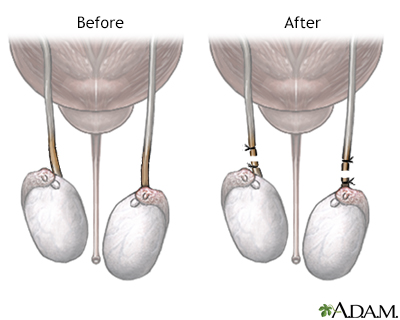 Before and after v...
Before and after v...
