Congenital heart surgery; Patent ductus arteriosus ligation; Hypoplastic left heart repair; Tetralogy of Fallot repair; Coarctation of the aorta repair; Atrial septal defect repair; Ventricular septal defect repair; Truncus arteriosus repair; Total anomalous pulmonary artery correction; Transposition of great vessels repair; Tricuspid atresia repair; VSD repair; ASD repair
Definition
Congenital heart defect corrective surgery fixes or treats a heart defect that a child is born with. A baby born with one or more heart defects has congenital heart disease. Surgery is needed if the defect could harm the child's long-term health or well-being. Sometimes, congenital heart disease is not detected until adulthood.
Description
There are many types of pediatric heart surgery.
Patent ductus arteriosus (PDA) ligation:
- Before birth, the baby has a blood vessel that runs between the aorta (the main artery to the body) and the pulmonary artery (the main artery to the lungs), called the ductus arteriosus. This small vessel most often closes shortly after birth when the baby starts to breathe on their own. If it does not close. It is called a patent ductus arteriosus. This could cause problems later in life.
- In most cases, the cardiologist will close off the opening using medicine. If this does not work, then other techniques are used.
- Sometimes the PDA can be closed with a procedure that does not involve surgery. The procedure is most often done in a laboratory that uses x-rays. In this procedure, the interventional cardiologist makes a small cut in the groin. A wire and tube called a catheter is inserted into an artery in the leg and passed up to the heart. Then, a small metal coil or another device is passed through the catheter into the infant's ductus arteriosus artery. The coil or other device blocks the blood flow, and this corrects the problem.
- Another method is to make a small surgical cut on the left side of the chest. The surgeon finds the PDA and then ties off or clips the ductus arteriosus, or divides and cuts it. Tying off the ductus arteriosus is called ligation. This procedure may be done in the neonatal intensive care unit (NICU).
Coarctation of the aorta repair:
- Coarctation of the aorta occurs when a part of the aorta has a very narrow section. The shape looks like an hourglass timer. The narrowing makes it difficult for blood to get through to the lower extremities. Over time, it can lead to problems such as extremely high blood pressure.
- To repair this defect, a cut is most often made on the left side of the chest, between the ribs. There are several ways to repair coarctation of the aorta.
- The most common way to repair it is to cut the narrow section and make it bigger with a patch made of GORE-TEX, a man-made (synthetic) material.
- Another way to repair this problem is to remove the narrow section of the aorta and stitch the remaining ends together. This can most often be done in older children.
- A third way to repair the problem is to connect a tube to the normal sections of the aorta, on either side of the narrow section. Blood flows through the tube and bypasses the narrow section.
- A newer method does not require surgery. An interventional cardiologist places a small wire through an artery in the groin and up to the aorta. A small balloon is then opened up in the narrow area of the aorta. A stent or small tube is left there to help keep the aorta open. The procedure is done in a laboratory with x-rays. This procedure is often used when the coarctation reoccurs after it has been fixed.
Atrial septal defect (ASD) repair:
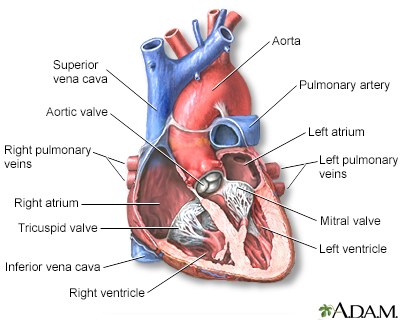
- The atrial septum is the wall between the left and right atria (upper chambers) of the heart. A hole in that wall is called an ASD. In the presence of this defect, blood with and without oxygen can be mixed up over time, causing medical problems and arrhythmias.
- Sometimes, an ASD can be closed without open-heart surgery. First, the interventional cardiologist makes a tiny cut in the groin. Then they insert a wire into a blood vessel that goes to the heart. Next, two small umbrella-shaped "clamshell" devices are placed on the right and left sides of the septum. These two devices are attached to each other. This closes the hole in the heart. Not all medical centers do this procedure.
- Open-heart surgery may also be done to repair ASD. In this operation, the septum can be closed using stitches. Another way to cover the hole is with a patch.
Ventricular septal defect (VSD) repair:
- The ventricular septum is the wall between the left and right ventricles (lower chambers) of the heart. A hole in the ventricular septum is called a VSD. This hole lets blood with oxygen mix with used blood (that has a low oxygen level)
returning to the lungs. Over time, irregular heartbeats and other heart problems can happen.
- By age 1, most small VSDs close on their own. However, those VSDs that do stay open after this age may need to be closed with surgery.
- Larger VSDs and small ones in certain parts of the ventricular septum, or ones that cause heart failure or endocarditis, (infection) need open-heart surgery. The hole in the septum is most often closed with a patch.
- Some septal defects can be closed without surgery. The procedure involves passing a small wire into the heart and placing a small device to close the defect.
Tetralogy of Fallot repair:
- Tetralogy of Fallot is a heart defect that usually includes four defects in the heart and causes the baby to turn a bluish color (cyanosis).
- Open-heart surgery is needed, and it is often done when the child is 6 months to 2 years old.
- The surgery involves closing the VSD with a patch and opening the thickened muscle (stenosis). A patch is placed on the right ventricle and main pulmonary artery to improve blood flow to the lungs.
- The child may have a shunt procedure done first. A shunt moves blood from one area to another. This is done if the open-heart surgery needs to be delayed because the child is too sick to go through surgery.
- Once the child is older, the shunt is closed and the main repair in the heart is performed.
Transposition of the great vessels repair:
- In a normal heart, the aorta comes from the left side of the heart, and the pulmonary artery comes from the right side. In children with transposition of the great vessels, these arteries come from the opposite sides of the heart. The child may also have other birth defects.
- Correcting transposition of the great vessels requires open-heart surgery. If possible, this surgery is done shortly after birth.
- The most common repair is called an arterial switch. The aorta and pulmonary artery are divided. The pulmonary artery is connected to the right ventricle, where it belongs. Then, the aorta and coronary arteries are connected to the left ventricle, where they belong.
Truncus arteriosus repair:
- Truncus arteriosus is a rare condition that occurs when the aorta, coronary arteries, and pulmonary artery all come out of one common trunk from the heart. The disorder may be very simple, or very complex. In all cases, it requires open-heart surgery to repair the defect.
- Repair is usually done in the first few days or weeks of the infant's life. The pulmonary arteries are separated from the aortic trunk, and any defects are patched. Usually, children also have a ventricular septal defect, and that is also closed. A connection is then placed between the right ventricle and the pulmonary arteries.
- Some children may need one or two more surgeries as they grow.
Tricuspid atresia repair:
- The tricuspid valve is between the upper and lower chambers on the right side of the heart. Tricuspid atresia occurs when this valve is deformed, narrow, or missing.
- Babies born with tricuspid atresia are blue because they cannot get blood to the lungs to pick up oxygen.
- To get to the lungs, blood must cross an atrial septal defect (ASD), ventricular septal defect (VSD), or a patent ductus arteriosus (PDA). (These conditions are described above.) This condition severely restricts blood flow to the lungs.
- Soon after birth, the baby may be given a medicine called prostaglandin E. This medicine will help keep the patent ductus arteriosus open so that blood can continue to flow to the lungs. However, this will only work for a while. The child will eventually need surgery.
- The child may need a series of shunts and surgeries to correct this defect. The goal of this surgery is to allow blood from the body to flow into the lungs. The surgeon may have to repair the tricuspid valve, replace the valve, or put in a shunt so that blood can get to the lungs.
Total anomalous pulmonary venous return (TAPVR) correction:
- TAPVR occurs when the pulmonary veins bring oxygen-rich blood from the lungs back to the right side of the heart, instead of the left side of the heart, where it most often goes in healthy people.
- This condition must be corrected with surgery. The surgery may be done in the newborn period if the infant has severe symptoms. If it is not done right after birth, it is done in the first 6 months of the baby's life.
- TAPVR repair requires open-heart surgery. The pulmonary veins are routed back to the left side of the heart, where they belong, and any abnormal connections are closed.
- If a PDA is present, it is tied off and divided.
Hypoplastic left heart repair:
- This is a very severe heart defect that is caused by a very poorly developed left heart. If it is not treated, it causes death in most babies who are born with it. Unlike babies with other heart defects, those with hypoplastic left heart do not have any other defects. Operations to treat this defect are done at specialized medical centers. Usually, surgery corrects this defect.
- A series of three heart operations is most often needed. The first operation is done in the first week of the baby's life. This is a complicated surgery where one blood vessel is created from the pulmonary artery and the aorta. This new vessel carries blood to the lungs and the rest of the body.
- The second operation, called a hemi-Fontan (HF) or Glenn procedure is most often done when the baby is 4 to 6 months old.
- The third operation, called a Fontan procedure, is most often done when a child is 18 to 36 months old.
References
Bernstein D. General principles of treatment of congenital heart disease. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 483.
Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2019;73(12):e81-e192. PMID: 30121239 pubmed.ncbi.nlm.nih.gov/30121239/.
Valente AM, Dorfman AL, Babu-Narayan SV, Krieger EV. Congenital heart disease in the adolescent and adult. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 82.
Well A, Fraser CD. Congenital heart disease. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 59.

 Heart - section th...
Heart - section th...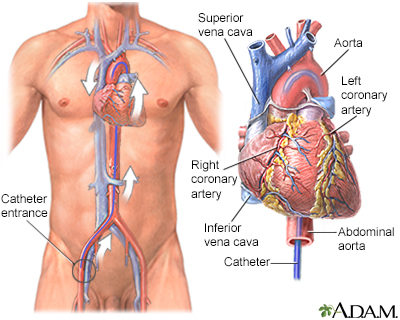 Cardiac catheteriz...
Cardiac catheteriz...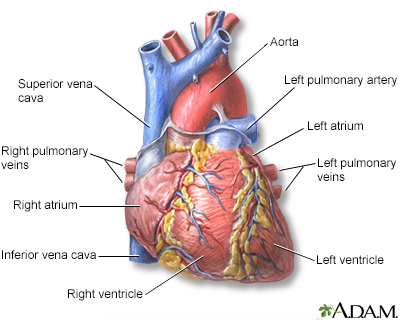 Heart - front view
Heart - front view Ultrasound, normal...
Ultrasound, normal...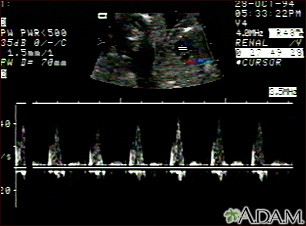 Ultrasound, ventri...
Ultrasound, ventri...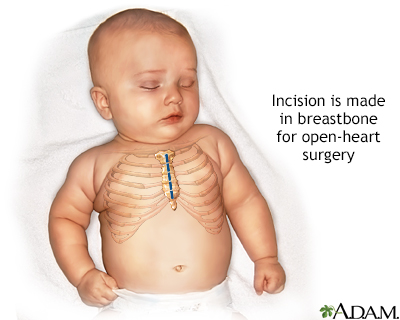 Infant open heart ...
Infant open heart ...
