Pregnancy SmartSiteTM
Skin transplant; Skin autografting; FTSG; STSG; Split thickness skin graft; Full thickness skin graft DefinitionA skin graft is a patch of skin that is removed by surgery from one area of the body and transplanted, or attached, to another area. DescriptionThis surgery is usually done while you are under general anesthesia. That means you will be asleep and pain-free. Healthy skin is taken from a place on your body called the donor site. Most people who are having a skin graft have a split-thickness skin graft. This takes the two top layers of skin from the donor site (the epidermis) and the layer under the epidermis (the dermis). The donor site can be any area of the body. Most times, it is an area that is hidden by clothes, such as the buttock, back, or inner thigh. The graft is carefully spread on the bare area where it is being transplanted. It is held in place either by gentle pressure from a well-padded dressing that covers it, or by staples or a few small stitches. The donor-site area is covered with a sterile dressing for 3 to 5 days. People with deeper tissue loss, or in a cosmetic area such as the face, may need a full-thickness skin graft. This requires the entire thickness of skin from the donor site, not just the top two layers. A full-thickness skin graft is a more complicated procedure. Common donor sites for full-thickness skin grafts include the chest wall, neck, back, or abdominal wall. Why the Procedure Is PerformedSkin grafts may be recommended for:
Full-thickness grafts are sometimes done when a lot of tissue is lost. This can happen with open fractures of the lower leg, or after severe infections. RisksRisks for anesthesia and surgery in general are:
Risks for this surgery are:
Before the ProcedureTell your surgeon or nurse if:
Planning for your surgery:
During the week before your surgery:
On the day of surgery:
After the ProcedureYou should recover quickly after split-thickness skin grafting. Full-thickness grafts need a longer recovery time. If you received this kind of graft, you may need to stay in the hospital for recovery. After you are discharged from the hospital, follow instructions on how to care for your skin graft, including:
Outlook (Prognosis)Most skin grafts are successful, but some do not heal well. You may need additional procedures to get the desired result. ReferencesLoder S, Levi B, Clark A. Skin grafting. In: Gurtner GC, Pusic AL, eds. Plastic Surgery, Volume 1: Principles. 5th ed. Philadelphia, PA: Elsevier; 2024:chap 17. Padilla PL, Khoo KH, Ho T, Cole EL, Sirvent RZ, Phillips LG. Plastic surgery. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 69. Ratner D, Nayyar PM. Grafts. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 5th ed. Philadelphia, PA: Elsevier; 2025:chap 148. | |
| |
Review Date: 1/21/2025 Reviewed By: Jonas DeMuro, MD, Diplomate of the American Board of Surgery with added Qualifications in Surgical Critical Care, Assistant Professor of Surgery, Renaissance School of Medicine, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

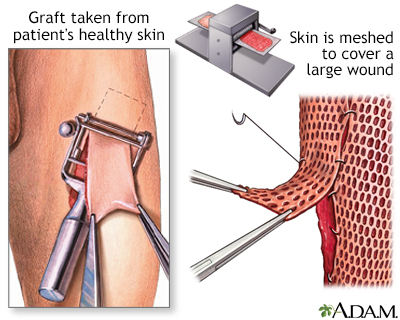 Skin graft
Skin graft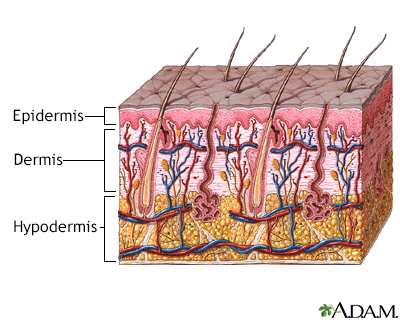 Skin layers
Skin layers
