Pregnancy SmartSiteTM
Cardiac transplant; Transplant - heart; Transplantation - heart DefinitionA heart transplant is surgery to remove a damaged or diseased heart and replace it with a healthy donor heart. DescriptionFinding a donor heart can be difficult. The heart must be donated by someone who is brain-dead but is still on life support. The donor heart must be in normal condition without disease and must be matched as closely as possible to your blood and tissue type to reduce the chance that your body will reject it. For this surgery, you are put into a deep sleep with general anesthesia, and a cut is made through the breastbone.
Why the Procedure Is PerformedA heart transplant may be done to treat:
Heart transplant surgery may not be used in people who:
RisksRisks from any anesthesia are:
Risks from any surgery are:
Risks of transplant include:
Before the ProcedureOnce you are referred to a transplant center, you will be evaluated by the transplant team. They will want to make sure that you are a good candidate for a transplant. You will visit many times over several weeks or even months. You will need to have blood drawn and x-rays taken. The following may also be done:
You will want to look at one or more transplant centers to see which would be best for you:
If the transplant team believes you are a good candidate, you will be put on a regional waiting list for a heart:
Most, but not all, people who are waiting for a heart transplant are very ill and need to be in the hospital. Many will need some sort of device to help their heart pump enough blood to the body. Most often, this is a ventricular assist device (VAD). After the ProcedureYou should expect to stay in the hospital for 7 to 21 days after a heart transplant. The first 24 to 48 hours will likely be in the intensive care unit (ICU). During the first few days after a transplant, you will need close follow-up to make sure that you do not get an infection and your heart is working well. The recovery period is about 3 months and often, your transplant team will ask you to stay fairly close to the hospital during that time period. You will need to have regular check-ups with blood tests, x-rays, and echocardiograms for many years. Fighting rejection is an ongoing process. The body's immune system considers the transplanted organ a foreign body and fights it. For this reason, organ transplant patients must take medicines that suppress the body's immune response. To prevent rejection, it is very important to take these medicines and carefully follow your self-care instructions. Biopsies of the heart muscle are often done every month during the first 6 to 12 months after transplant, and then less often after that. This helps determine if your body is rejecting the new heart, even before you have symptoms. You must take medicines that prevent transplant rejection for the rest of your life. You will need to understand how to take these medicines, and know their side effects. You can go back to your normal activities 3 months after the transplant as soon as you feel well enough, and after talking with your health care provider. Consult your provider if you plan to engage in vigorous physical activity. If you develop coronary disease after a transplant, you may have cardiac catheterization every year. Outlook (Prognosis)Heart transplant prolongs the life of people who would otherwise die. About 90% of heart transplant patients are alive 1 year after the operation. At 3 years, more than 85% of patients will still be alive after a heart transplant. The main problem, as with other transplants, is rejection. If rejection can be controlled, survival increases to over 10 years. ReferencesHeidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895–e1032. PMID: 35363499 pubmed.ncbi.nlm.nih.gov/35363499/. Kliegman RM, St. Geme JW, Blum NJ, et al. Pediatric heart and heart-lung transplantation. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philaelphia, PA: Elsevier; 2025:chap 492. McMurray JJV, Pfeffer MA. Heart failure: Treatment and prognosis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 46. Shudo Y, Hiesinger W, Woo YJ. Heart transplantation. In: Sellke FW, del Nido PJ, Swanson SJ, eds. Sabiston and Spencer Surgery of the Chest. 10th ed. Philadelphia, PA: Elsevier; 2024:chap 102. Starling RC. Cardiac transplantation. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 60. | |
| |
Review Date: 5/5/2025 Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

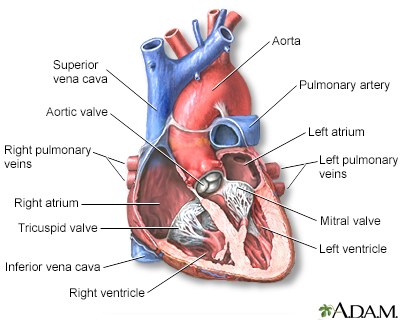 Heart - section th...
Heart - section th...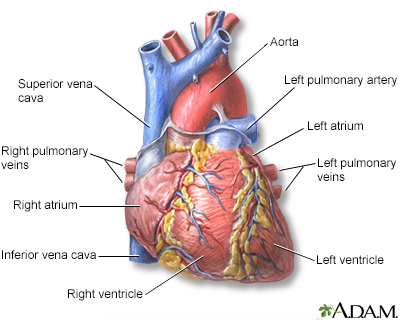 Heart - front view
Heart - front view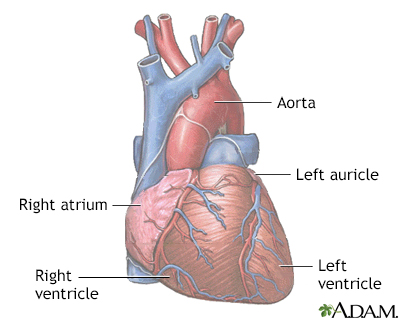 Normal anatomy of ...
Normal anatomy of ...
