Pregnancy SmartSiteTM
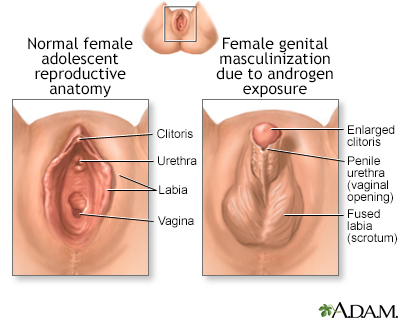
Genitals - ambiguous; Uncertain genitalia; Atypical genitalia DefinitionAmbiguous genitalia is a rare condition where a child is born with outer genitals that do not clearly look either male or female. They may have features of both sexes or not be fully developed. The characteristics of the child's genitals may not match their internal sex organs or their genetic sex. This condition is also called uncertain genitalia or atypical genitalia. Ambiguous genitalia is common in children with differences of sex development (DSD). ConsiderationsThe genetic sex of a child is determined at conception. The mother's egg cell contains an X chromosome, while the father's sperm cell contains either an X or a Y chromosome. These X and Y chromosomes determine the child's genetic sex. Normally, an infant inherits 1 pair of sex chromosomes, 1 X from the mother and 1 X or 1 Y from the father. A baby who inherits the X chromosome from the father has 2 X chromosomes and is a genetic female. A baby who inherits the Y chromosome from the father has 1 X and 1 Y chromosome and is a genetic male. The male and female reproductive organs and genitals both come from the same tissue in the fetus. Ambiguous genitalia can develop if the process that causes this fetal tissue to become "male" or "female" is disrupted. This means the external genitals do look clearly male or female or may have characteristics of both. The physical appearance of people with this condition can vary widely. Very rarely, the physical appearance may be fully developed as the opposite of the genetic sex. For example, a genetic male may have developed the appearance of a female. In most cases, ambiguous genitalia in genetic females (infants with 2 X chromosomes) has the following features:
In a genetic male (1 X and 1 Y chromosome), ambiguous genitalia most often include the following features: A small penis (less than 2 to 3 centimeters, or 3/4 to 1 1/4 inches) that looks like an enlarged clitoris (the clitoris of a newborn female is normally somewhat enlarged at birth). The urethral opening may be anywhere along, above, or below the penis (hypospadias). It can be located as low as the perineum, further making the infant appear to be female. There may be a small scrotum that is separated and looks like labia. Undescended testicles commonly occur with ambiguous genitalia. With a few exceptions, ambiguous genitalia is most often not life-threatening. However, its treatment has short- and long-term consequences. For this reason, a team of health care professionals with expertise in DSD will work together to understand and treat the child and support the family. This team may include neonatologists, geneticists, endocrinologists, and psychiatrists or social workers. The specific treatment will depend on the specific cause of the ambiguous genitalia. CausesCauses for ambiguous genitalia include:
Home Care
When to Contact a Medical ProfessionalContact your health care provider if you are concerned about the appearance of your child's external genitalia, or your baby:
These can all be signs of congenital adrenal hyperplasia. Ambiguous genitalia may be discovered during the first well-baby exam. What to Expect at Your Office VisitThe provider will perform a physical exam which may reveal genitals that are not "typical male" or "typical female," but somewhere in between. The provider will ask medical history questions to help identify any chromosomal disorders. Questions may include:
The following tests may be done:
Endoscopy, abdominal x-ray, abdominal or pelvic ultrasound, and similar tests may be needed to determine the presence or absence of the internal genitals (such as undescended testes). In some cases, laparoscopy, exploratory laparotomy, or biopsy of the gonads may be needed to confirm disorders that can cause ambiguous genitalia. Depending on the cause, surgery, hormone replacement, or other treatments are used to treat conditions that can cause ambiguous genitalia. There have been significant changes in treating ambiguous genitalia. In the past, the external genitals were prioritized over chromosomes. Expert opinion has shifted to understanding that chromosomal, neural, hormonal, psychological, and behavioral factors can all have an influence on an individual. Many experts now urge delaying definitive surgery for as long as is healthy, and ideally involving the child in the decision, unless surgery is needed for the health of the infant. Working with your child’s heath care team can help you make the best choices for your child. In addition, a DSD support group can help provide families with the latest research and offer a community of other families, children, and adult individuals who have faced the same issues. ReferencesFischer KM, Kolon TF. Embryology and differences of sex development. In: Guzzo TJ, Wein AJ, Kovell RC, Weiss DA, Ziemba JB, eds. Penn Clinical Manual of Urology. 3rd ed. Philadelphia, PA: Elsevier; 2024:chap 25. Vilain E, Shimy K. Differences of sex development. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 101. White PC. Congenital adrenal hyperplasia and related disorders. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 594. White PC. Sexual development and identity. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 214. Yu RN, Diamond DA. Disorders of sexual development: etiology, evaluation, and medical management. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 48. | |
| |
Review Date: 3/12/2024 Reviewed By: Anna C. Edens Hurst, MD, MS, Associate Professor in Medical Genetics, The University of Alabama at Birmingham, Birmingham, AL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 02/05/2025. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Developmental diso...
Developmental diso...
