Pregnancy SmartSiteTM
Joint hypermobility; Loose joints; Hypermobility syndrome DefinitionHypermobile joints are joints that move beyond the normal range with little effort. Joints most commonly affected are the elbows, wrists, fingers, and knees. ConsiderationsChildren's joints are often more flexible than adults' joints. But children with hypermobile joints can flex and extend their joints beyond what is considered normal. The movement is done without too much force and without discomfort. Thick bands of tissue called ligaments help hold joints together and keep them from moving too much or too far. In children with hypermobility syndrome, those ligaments are loose or weak. This may lead to:
Children with hypermobile joints also often have flat feet. CausesHypermobile joints often occur in otherwise healthy and normal children. This is called benign hypermobility syndrome. Rare medical conditions associated with hypermobile joints include:
Home CareThere is no specific care for this condition. People with hypermobile joints have an increased risk for joint dislocation and other problems. Extra care may be needed to protect the joints. Ask your health care provider for recommendations. When to Contact a Medical ProfessionalContact your provider if:
What to Expect at Your Office VisitHypermobile joints often occur with other symptoms that, taken together, define a specific syndrome or condition. A diagnosis is based on a family history, your medical history, and a complete physical exam. The exam includes a close look at your muscles and bones. Your provider will ask about the symptoms, including:
Further tests may be done. ReferencesBall JW, Dains JE, Flynn JA, Solomon BS, Stewart RW. Musculoskeletal system. In: Ball JW, Dains JE, Flynn JA, Solomon BS, Stewart RW, eds. Seidel's Guide to Physical Examination. 10th ed. St Louis, MO: Elsevier; 2023:chap 22. Clinch J, Rogers VJ. Hypermobility syndrome. In: Hochberg MC, Gravallese EM, Smolen JS, van der Heijde D, Weinblatt ME, Weisman MH, eds. Rheumatology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 217. | |
| |
Review Date: 10/20/2024 Reviewed By: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

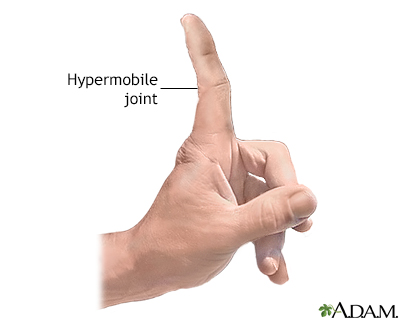 Hypermobile joints
Hypermobile joints
