Pregnancy SmartSiteTM
Funnel chest; Cobbler's chest; Sunken chest DefinitionPectus excavatum is a medical term that describes an abnormal formation of the rib cage that gives the chest a caved-in or sunken appearance. ConsiderationsPectus excavatum occurs while a baby is developing in the womb. It can also develop in a baby after birth. The condition can be mild or severe. Pectus excavatum is due to too much growth of the connective tissue that joins the ribs to the breastbone (sternum). This causes the sternum to grow inward. As a result, there is a depression in the chest over the sternum, which may appear quite deep. If the condition is severe, the heart and lungs can be affected. Also, the way the chest looks may cause emotional stress for the child. CausesThe exact cause is unknown. Pectus excavatum may occur by itself. Or there may be a family history of the condition. Other medical problems linked with this condition include:
When to Contact a Medical ProfessionalContact your health care provider if you or your child has any of the following:
What to Expect at Your Office VisitYour provider will perform a physical examination. An infant with pectus excavatum may have other symptoms and signs that, when taken together, define a specific condition known as a syndrome. Your provider will also ask about medical history, such as:
Tests may be done to rule out suspected disorders. These tests may include:
Tests may also be done to find out how severely the lungs and heart are affected. This condition can be surgically repaired. Surgery is generally advised if there are other health problems, such as trouble breathing. Surgery may also be done to improve the appearance of the chest. Talk to your provider about treatment options. ReferencesBeh HZ, Ferry AM, Dibbs RP, Buchanan EP, Monson LA. Pediatric chest and trunk deformities. In: Losee JE, Hopper RA, eds. Plastic Surgery: Volume 3: Craniofacial, Head and Neck Surgery and Pediatric Plastic Surgery. 5th ed. Philadelphia, PA: Elsevier; 2024:chap 32. Boas SR. Skeletal diseases influencing pulmonary function. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 445. Weller JH, Nasr IW. Repair of pectus excavatum. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:951-992. | |
| |
Review Date: 8/22/2023 Reviewed By: Mary C. Mancini, MD, PhD, Cardiothoracic Surgeon, Shreveport, LA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

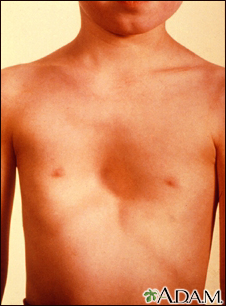 Pectus excavatum
Pectus excavatum Ribcage
Ribcage
