Pregnancy SmartSiteTM
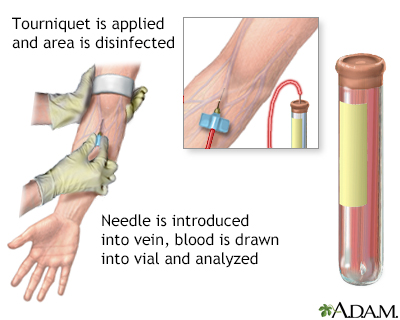
CP - serum; Copper - ceruloplasmin DefinitionThe ceruloplasmin test measures the level of the copper-containing protein ceruloplasmin in the blood. How the Test is PerformedA blood sample is needed. How to Prepare for the TestNo special preparation is needed. How the Test will FeelWhen the needle is inserted to draw blood, some people feel moderate pain. Others feel only a prick or stinging. Afterward, there may be some throbbing or a slight bruise. This soon goes away. Why the Test is PerformedCeruloplasmin is made in the liver. Ceruloplasmin stores and transports copper in the blood to parts of the body that need it. Your health care provider may order this test if you have signs or symptoms of a copper metabolism or copper storage disorder. Normal ResultsThe normal range for adults is 20 to 40 mg/dL. Normal value ranges may vary slightly among different labs. Some labs use different measurements or may test different samples. Talk to your provider about the meaning of your specific test results. What Abnormal Results MeanA lower-than-normal ceruloplasmin level may be due to:
A higher-than-normal ceruloplasmin level may be due to:
RisksThere is little risk in having your blood taken. Veins and arteries vary in size from one person to another, and from one side of the body to the other. Obtaining a blood sample from some people may be more difficult than from others. Other risks associated with having blood drawn are slight, but may include:
ReferencesKoppel BS, Weimer LH, Daras M. Nutritional and alcohol-related neurologic disorders. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 384. McPherson RA. Specific proteins. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 24th ed. Philadelphia, PA: Elsevier; 2022:chap 20. Schilsky ML. Wilson disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 195. | |
| |
Review Date: 2/13/2025 Reviewed By: Jacob Berman, MD, MPH, Clinical Assistant Professor of Medicine, Division of General Internal Medicine, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Blood test
Blood test
