Pregnancy SmartSiteTM
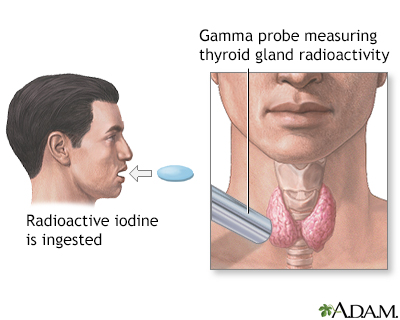
Thyroid uptake; Iodine uptake test; RAIU DefinitionRadioactive iodine uptake (RAIU) tests thyroid function. It measures how much radioactive iodine is taken up by your thyroid gland in a certain time period. A similar test is the thyroid scan. The 2 tests are commonly performed together, but they can be done separately. How the Test is PerformedThe test is done in this way:
The test takes less than 30 minutes, but you will need to come back twice to have the scans performed. How to Prepare for the TestFollow instructions about not eating before the test. You may be told not to eat after midnight the night before your test. Your health care provider will tell you if you need to stop taking medicines before the test that may affect your test results. Do not stop taking any medicine without first talking to your provider. Tell your provider if you have:
How the Test will FeelThere is no discomfort. You can eat beginning about 1 to 2 hours after swallowing the radioactive iodine. You can go back to a normal diet after the test. Why the Test is PerformedThis test is done to check thyroid function. It is often done when blood tests of thyroid function show that you may have an overactive thyroid gland. Normal ResultsThese are normal results at 6 and 24 hours after swallowing the radioactive iodine:
Some testing centers measure only at 24 hours. Values may vary depending on the amount of iodine in your diet. Normal value ranges may vary slightly among different labs. Talk to your provider about the meaning of your specific test results. What Abnormal Results MeanHigher-than-normal uptake may be due to an overactive thyroid gland. The most common cause is Graves disease. Other conditions can cause some areas of higher-than-normal uptake in the thyroid gland. These include:
These conditions often result in normal uptake, but the uptake is concentrated into a few (hot) areas while the rest of the thyroid gland does not take up any iodine (cold areas). This can only be determined if the scan is done along with the uptake test. Lower-than-normal uptake may be due to:
RisksAll radiation has possible side effects. The amount of radiation in this test is very small, and there have been no documented side effects. Women who are pregnant or breastfeeding should not have this test. Talk to your provider if you have concerns about this test. ConsiderationsThe radioactive iodine leaves your body through your urine. You need not take special precautions, such as flushing twice after urinating, for 24 to 48 hours after the test because the dose of radioactive iodine is very low. Ask your provider or the radiology/nuclear medicine team performing the scan about taking precautions. ReferencesFaix JD. Thyroid function testing (thyrotropin, triiodothyronine, and thyroxine). In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 68. Guber HA, Oprea M, Rusell YX. Evaluation of endocrine function. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 24th ed. Philadelphia, PA: Elsevier; 2022:chap 25. Mettler FA, Guiberteau MJ. Thyroid, parathyroid, and salivary glands. In: Mettler FA, Guiberteau MJ, eds. Essentials of Nuclear Medicine and Molecular Imaging. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 4. Salvatore D, Cohen R, Kopp PA, Larsen PR. Thyroid pathophysiology and diagnostic evaluation. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 11. | |
| |
Review Date: 2/28/2024 Reviewed By: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Thyroid uptake tes
Thyroid uptake tes
