Pregnancy SmartSiteTM
V/Q scan; Ventilation/perfusion scan; Lung ventilation/perfusion scan; Pulmonary embolism - V/Q scan; PE- V/Q scan; Blood clot - V/Q scan DefinitionA pulmonary ventilation/perfusion scan involves two nuclear scan tests to measure breathing (ventilation) and circulation (perfusion) in all areas of the lungs. How the Test is PerformedA pulmonary ventilation/perfusion scan is actually 2 tests. They may be done separately or together. During the perfusion scan, a technician injects radioactive albumin into your vein. You are placed on a movable table that is under the arm of a scanner. The machine scans your lungs as blood flows through them to find the location of the radioactive particles. During the ventilation scan, you breathe in radioactive gas through a mask while you are sitting or lying on a table under the scanner arm. How to Prepare for the TestYou do not need to stop eating (fast), be on a special diet, or take any medicines before the test. A chest x-ray is usually done before, and sometimes after a ventilation and perfusion scan. You wear a hospital gown or comfortable clothing that does not have metal fasteners. How the Test will FeelThe table may feel hard or cold. You may feel a sharp prick when the IV is placed in the vein in your arm for the perfusion part of the scan. The mask used during the ventilation scan may make you feel nervous about being in a small space (claustrophobia). You must lie still during the scan. The radioisotope injection usually does not cause discomfort. Why the Test is PerformedThe ventilation scan is used to see how well air moves and blood flows through the lungs. The perfusion scan measures the blood supply through the lungs. A ventilation and perfusion scan is most often done to detect an acute pulmonary embolus (blood clot in the lungs). It is also used to:
Normal ResultsA radiologist will evaluate your ventilation and perfusion scan in conjunction with a chest x-ray. All parts of both lungs should take up the radioisotope evenly. What Abnormal Results MeanIf the lungs take up lower than normal amounts of radioisotope during a ventilation or perfusion scan, it may be due to any of the following:
RisksRisks are about the same as for x-rays (radiation) and needle pricks. No radiation is released from the scanner. Instead, it detects radiation and converts it into an image. There is a small exposure to radiation from the radioisotope. The radioisotopes used during scans are short-lived. All of the radiation leaves the body in a few days. However, as with any radiation exposure, caution is advised for pregnant or breastfeeding women. There is a slight risk for infection or bleeding at the site where the needle is inserted. The risk with perfusion scan is the same as with inserting an intravenous needle for any other purpose. In rare cases, a person may develop an allergy to the radioisotope. This may include a serious anaphylactic reaction. ConsiderationsA pulmonary ventilation and perfusion scan may be a lower-risk alternative to pulmonary angiography for evaluating disorders of the lung blood supply. This test may not provide a definite diagnosis, particularly in people with lung disease. Other tests may be needed to confirm or check for the findings of a pulmonary ventilation and perfusion scan. This test has largely been replaced by CT pulmonary angiography for diagnosing pulmonary embolism. However, people with kidney problems or an allergy to contrast dye can more safely have this test. ReferencesHerring W. Nuclear medicine: understanding the principles and recognizing the basics. In: Herring W, ed. Learning Radiology: Recognizing the Basics. 5th ed. Philadelphia, PA: Elsevier; 2024:e Appendix e1-e20. Morris TA, Rose A. Pulmonary thromboembolism: presentation and diagnosis. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 81. Nair A, Barnett JL, Semple TR. Current status of thoracic imaging. In: Adam A, Dixon AK, Gillard JH, Schaefer-Prokop CM, eds. Grainger & Allison's Diagnostic Radiology. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 1. | |
| |
Review Date: 8/19/2024 Reviewed By: Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutgers New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

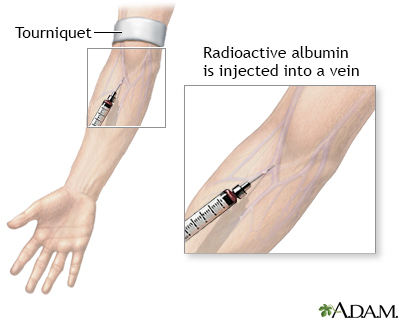 Albumin injection
Albumin injection
