Pregnancy SmartSiteTM
Esophagogastroduodenoscopy; Upper endoscopy; Gastroscopy; EGD DefinitionEsophagogastroduodenoscopy (EGD) is a test to examine the lining of the esophagus, stomach, and first part of the small intestine (the duodenum). How the Test is PerformedEGD is done in a hospital or outpatient center by a specially trained doctor called a gastroenterologist. The procedure uses an endoscope. This is a flexible tube with a light and camera at the end. The procedure is done as follows:
After the test is finished, you will not be able to have food and liquid until your gag reflex returns (so you do not choke). The test lasts about 5 to 20 minutes. Follow any instructions you're given for recovering at home. How to Prepare for the TestYou will not be able to eat anything for 6 to 12 hours before the test. Follow instructions about stopping aspirin and other blood-thinning medicines before the test. How the Test will FeelThe anesthetic spray makes it hard to swallow. This wears off shortly after the procedure. The scope may make you gag. You may feel gas and the movement of the scope in your abdomen. You will not be able to feel the biopsy. Because of sedation, you may not feel any discomfort and have no memory of the test. You may feel bloated from the air that was put into your body. This feeling soon wears off. Why the Test is PerformedEGD may be done if you have symptoms that are new, cannot be explained, or are not responding to treatment, such as:
Your health care provider may also order this test if you:
The test may also be used to take a piece of tissue for biopsy. Normal ResultsThe esophagus, stomach, and duodenum should be smooth and of normal color. There should be no bleeding, growths, ulcers, or inflammation. What Abnormal Results MeanAn abnormal EGD may be the result of:
RisksThere is a small chance of a hole (perforation) in the stomach, duodenum, or esophagus from the scope moving through these areas. There is also a small risk of bleeding at the biopsy site. You could have a reaction to the medicine used during the procedure, which could cause:
ReferencesKoch MA, Zurad EG. Esophagogastroduodenoscopy. In: Fowler GC, ed. Pfenninger & Fowler's Procedures for Primary Care. 4th ed. Philadelphia, PA: Elsevier; 2020:chap 91. Sugumar A, Vargo JJ. Preparation for and complications of gastrointestinal endoscopy. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 42. | |
| |
Review Date: 8/7/2023 Reviewed By: Michael M. Phillips, MD, Emeritus Professor of Medicine, The George Washington University School of Medicine, Washington, DC. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

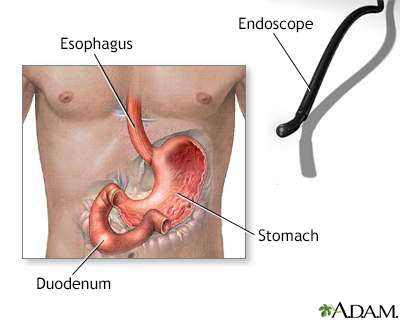 Gastric endoscopy
Gastric endoscopy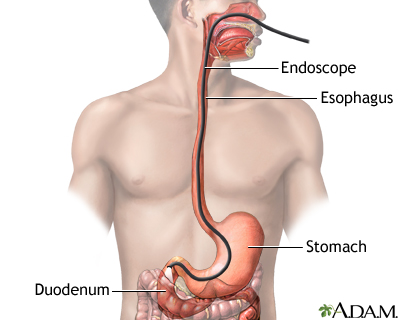 Esophagogastroduod...
Esophagogastroduod...
