Pregnancy SmartSiteTM
Sleep study; Polysomnogram; Rapid eye movement studies; Split night polysomnography; PSG; OSA - sleep study; Obstructive sleep apnea - sleep study; Sleep apnea - sleep study DefinitionPolysomnography is a sleep study. This test records certain body functions as you sleep, or try to sleep. Polysomnography is used to diagnose sleep disorders. How the Test is PerformedThere are two types of sleep:
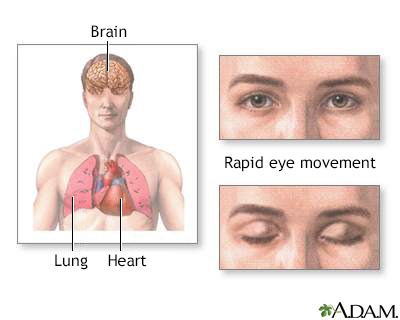
REM sleep alternates with NREM sleep about every 90 minutes. A person with normal sleep most often has four to five cycles of REM and NREM sleep during a night. A sleep study measures your sleep cycles and stages by recording:
Polysomnography can be done either at a sleep center or in your home. AT A SLEEP CENTER Full sleep studies are most often done at a special sleep center.
AT HOME You may be able to use a sleep study device in your home instead of at a sleep center to help diagnose sleep apnea. You either pick up the device at a sleep center or a trained therapist comes to your home to set it up. Many sleep centers may also have a mail-to-home option so that the device can be delivered to your doorstep. Home testing may be used when:
How to Prepare for the TestWhether the test is at a sleep study center or at home, you prepare the same way. Unless directed to do so by your sleep specialist, do not take any sleep medicine and do not drink alcohol or caffeinated beverages before the test. They can interfere with your sleep. Why the Test is PerformedThe test helps diagnose possible sleep disorders, including obstructive sleep apnea (OSA). Your health care provider may think you have OSA because you have these symptoms:
Polysomnography can also diagnose other sleep disorders:
Normal ResultsA sleep study tracks:
Most people have short periods during sleep where their breathing stops or is partly blocked. The apnea-hypopnea index (AHI) is the number of apnea or hypopnea episodes that occur per hour measured during a sleep study. AHI results are used to diagnose obstructive or central sleep apnea. Normal test results show:
What Abnormal Results MeanIn adults, an apnea-hypopnea index (AHI) of 5 per hour or above may mean you have sleep apnea:
To make a diagnosis and decide on treatment, your sleep specialist must also look at:
ReferencesAvidan AY. Sleep and its disorders. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 101. Kirk V, Baughn J, D'Andrea L, et al. American Academy of Sleep Medicine position paper for the use of a home sleep apnea test for the diagnosis of OSA in children. J Clin Sleep Med. 2017;13(10):1199-1203. PMID: 28877820 pubmed.ncbi.nlm.nih.gov/28877820/. Sarber KM, Lam DJ, Ishman SL. Sleep apnea and sleep disorders. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 15. Shangold L. Clinical polysomnography. In: Friedman M, Jacobowitz O, eds. Sleep Apnea and Snoring. 2nd ed. Philadelphia, PA: Elsevier; 2020:chap 4. | |
| |
Review Date: 5/3/2024 Reviewed By: Allen J. Blaivas, DO, Division of Pulmonary, Critical Care, and Sleep Medicine, VA New Jersey Health Care System, Clinical Assistant Professor, Rutgers New Jersey Medical School, East Orange, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Sleep studies
Sleep studies
