Pregnancy SmartSiteTM
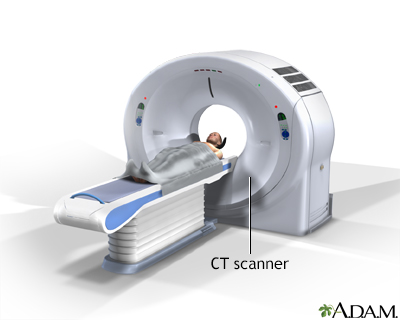
Colonoscopy - virtual; CT colonography; Computed tomographic colonography; Colography - virtual DefinitionA virtual colonoscopy (VC) is an imaging or x-ray test that looks for cancer, polyps, or other disease in the large intestine (colon). The medical name of this test is CT colonography. How the Test is PerformedA VC is different from a regular colonoscopy. A regular colonoscopy uses a long, lighted tool called a colonoscope that is inserted into the rectum and large intestine. A VC is done in the radiology department of a hospital or medical center. No sedatives are needed and no colonoscope is used. The exam is done as follows:
A computer combines all the images to form three-dimensional pictures of the colon. The radiologist can view the images on a video monitor. How to Prepare for the TestYour bowels need to be completely empty and clean for the exam. A problem in your large intestine that needs to be treated may be missed if your intestines are not cleaned out. Your health care provider will give you the steps for cleansing your bowel. This is called bowel preparation. Steps may include:
You need to drink plenty of clear liquids for 1 to 3 days before the test. Examples of clear liquids are:
Keep taking your medicines unless your provider tells you otherwise. You will need to stop taking iron pills or liquids a few days before the test, unless your provider tells you it is OK to continue. Iron can make your stool dark black. This makes it harder for the radiologist to view inside your bowel. CT scanners are very sensitive to metals. Do not wear jewelry the day of your exam. You will be asked to change out of your street clothes and wear a hospital gown for the procedure. How the Test will FeelThe x-rays are painless. Pumping air into the colon may cause cramping or gas pains. After the exam:
Why the Test is PerformedVC may be done for the following reasons:
Your provider may recommend a regular colonoscopy instead of a VC. One reason is that VC does not allow removing tissue samples or polyps. It does not allow treatment of any problems discovered. Another reason is that CT scans require radiation, which a colonoscopy does not. This is particularly true if virtual colonoscopy is to be performed multiple times at the recommended every 5 years. Colonoscopy is the preferred test in people who have had colon polyps, colon cancer, or are at higher risk of these because of other conditions. Normal ResultsNormal findings are images that show a healthy intestinal tract. What Abnormal Results MeanAbnormal test results may mean any of the following:
A regular colonoscopy may be done (on a different day) after a VC if:
RisksRisks of a VC include:
ConsiderationsThe differences between a virtual and a conventional colonoscopy include:
ReferencesGarber JJ, Chung DC. Colonic polyps and polyposis syndromes. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology Diagnosis Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 126. Kim DH, Pickhardt PJ. Computed tomography colonography and evaluation of the colon. In: Gore RM, Levine MS, eds. Textbook of Gastrointestinal Radiology. 5th ed. Philadelphia, PA: Elsevier; 2021:chap 38. Lawler M, Johnston B, Van Schaeybroeck S, et al. Colorectal cancer. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 74. National Cancer Institute website. Colorectal cancer prevention (PDQ) - health professional version. www.cancer.gov/types/colorectal/hp/colorectal-prevention-pdq. Updated April 11, 2025. Accessed August 12, 2025. National Comprehensive Cancer Network website. NCCN clinical practice guidelines in oncology (NCCN guidelines): colorectal cancer screening. Version 2.2025 - June 24, 2025. www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf. Updated June 24, 2025. Accessed August 12, 2025. Patel SG, May FP, Anderson JC, et al. Updates on age to start and stop colorectal cancer screening: recommendations from the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022;162(1):285-299. PMID: 34794816 pubmed.ncbi.nlm.nih.gov/34794816/. Shaukat A, Kahi CJ, Burke CA, Rabeneck L, Sauer BG, Rex DK. ACG clinical guidelines: colorectal cancer screening 2021. Am J Gastroenterol. 2021;116(3):458-479. PMID: 33657038 pubmed.ncbi.nlm.nih.gov/33657038/. US Preventive Services Task Force website. Final recommendation statement. Colorectal cancer: screening. www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening. Published May 18, 2021. Accessed April 6, 2025. | |
| |
Review Date: 2/3/2025 Reviewed By: Jenifer K. Lehrer, MD, Gastroenterologist, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 08/12/2025. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 CT scan
CT scan
