Pregnancy SmartSiteTM
Intrinsic sphincter deficiency repair; ISD repair; Injectable bulking agents for stress urinary incontinence DefinitionInjectable implants are injections of material into the wall of the urethra to help control urine leakage (urinary incontinence) caused by a weak urinary sphincter. The sphincter is a muscle that allows your body to hold urine in the bladder. If your sphincter muscle stops working well, you will have urine leakage. DescriptionThe material that is injected is permanent. Coaptite and Macroplastique are examples of two brands. The surgeon injects material through a needle into the wall of your urethra. This is the tube that carries urine from your bladder out of your body. The material bulks up the urethral tissue, causing it to tighten. This stops urine from leaking out of your bladder. You may receive one of the following types of anesthesia (pain relief) for this procedure:
After you are numb or asleep from anesthesia, the surgeon puts a medical device called a cystoscope into your urethra. The cystoscope allows your surgeon to see the area. Then the surgeon passes a needle through the cystoscope into your urethra. Material is injected into the wall of the urethra or bladder neck through this needle. The surgeon can also inject material into the tissue next to the sphincter. The implant procedure is usually done in the hospital. Or, it is done in your surgeon's office. The procedure takes about 20 to 30 minutes. Why the Procedure Is PerformedImplants can help both men and women. Men who have urine leakage after prostate surgery may choose to have implants. Women who have urine leakage and want a simple procedure to control the problem may choose to have an implant procedure. These women may not want to have surgery that requires general anesthesia or a long recovery after surgery. RisksRisks for this procedure are:
Before the ProcedureTell your surgeon what medicines you are taking. This includes medicines, supplements, or herbs you bought without a prescription. You may be asked to stop taking aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), vitamin E, warfarin (Coumadin), and any other medicines that make it hard for your blood to clot (blood thinners). On the day of your procedure:
After the ProcedureMost people can go home soon after the procedure. It may take up to a month before the injection fully works. It may become harder to empty your bladder. You may need to use a catheter for a few days. This and any other urinary problems usually go away. Outlook (Prognosis)You may need 2 or 3 more injections to get good results. If the material moves away from the spot where it was injected, you may need more treatments in the future. Implants can help most men who have had transurethral resection of the prostate (TURP). Implants help about one half of men who have had their prostate gland removed to treat prostate cancer. ReferencesBoone TB, Stewart JN, Martinez LM. Additional therapies for storage and emptying failure. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 127. Kobashi KC, Vasavada S, Bloschichak A, et al. Updates to surgical treatment of female stress urinary incontinence (SUI): AUA/SUFU Guideline (2023). J Urol. 2023;209(6):1091-1098. PMID: 37096580 pubmed.ncbi.nlm.nih.gov/37096580/. Lentz GM, Miller JL. Lower urinary tract function and disorders: physiology of micturition, voiding dysfunction, urinary incontinence, urinary tract infections, and painful bladder syndrome. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 21. | |
| |
Review Date: 1/1/2025 Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

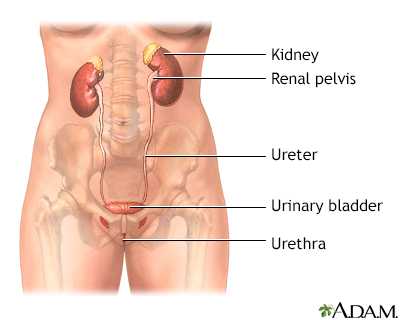 Female urinary tra...
Female urinary tra...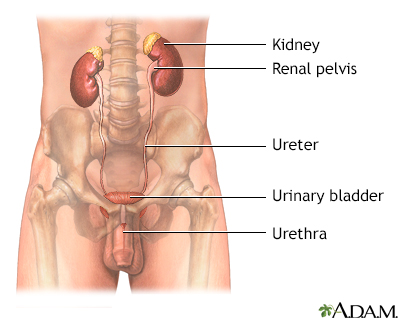 Male urinary tract
Male urinary tract
