Pregnancy SmartSiteTM
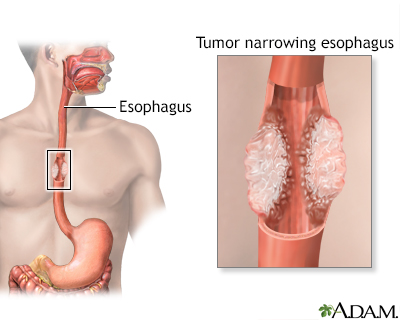
Minimally invasive esophagectomy; Robotic esophagectomy; Removal of the esophagus - minimally invasive; Achalasia - esophagectomy; Barrett esophagus - esophagectomy; Esophageal cancer - esophagectomy - laparoscopic; Cancer of the esophagus - esophagectomy - laparoscopic DefinitionMinimally invasive esophagectomy is surgery to remove part or all of the esophagus. This is the tube that moves food from your throat to your stomach. After it is removed, the esophagus is rebuilt from part of your stomach or part of your large intestine. Most of the time, esophagectomy is done to treat cancer of the esophagus. The surgery may also be done to treat the esophagus if it is no longer working to move food into the stomach. DescriptionDuring minimally invasive esophagectomy, small surgical cuts (incisions) are made in your upper belly, chest, or neck. A viewing scope (laparoscope) and surgical tools are inserted through the incisions to perform the surgery. (Removal of the esophagus can also be done using the open method. Surgery is done through larger incisions.) Laparoscopic surgery is generally done in the following way:
Some medical centers do this operation using robotic surgery. In this type of surgery, a small scope and other instruments are inserted through the small cuts in the skin. The surgeon controls the scope and instruments while sitting at a computer station and viewing a monitor. Surgery usually takes 3 to 6 hours. Why the Procedure Is PerformedThe most common reason for removing part, or all, of your esophagus is to treat cancer of the esophagus. You may also have radiation therapy or chemotherapy before or after surgery. Surgery to remove the lower esophagus may also be done to treat:
RisksThis is major surgery and has many risks. Some of them are serious. Be sure to discuss these risks with your surgeon. Risks for this surgery, or for problems after surgery, may be higher than normal if you:
Risks for anesthesia and surgery in general are:
Risks for this surgery are:
Before the ProcedureYou will have many medical visits and tests before you have surgery. Some of these are:
If you are a smoker, you should stop several weeks before surgery. Ask your provider for help. Tell your surgeon or nurse if:
During the week before your surgery:
On the day of surgery:
After the ProcedureMost people stay in the hospital for 7 to 14 days after an esophagectomy. How long you stay will depend on what type of surgery you had. You may spend 1 to 3 days in the intensive care unit (ICU) right after surgery. During your hospital stay, you will:
After you go home, follow instructions on how to take care of yourself as you heal. You'll be given information on diet and eating. Be sure to follow those instructions as well. Outlook (Prognosis)Many people recover well from this surgery and can have a fairly normal diet. After they recover, they will likely need to eat smaller portions and eat more often. If you had the surgery for cancer, talk with your provider about the next steps to treat the cancer. ReferencesNational Cancer Institute website. Esophageal cancer treatment (PDQ) - health professional version. www.cancer.gov/types/esophageal/hp/esophageal-treatment-pdq. Updated March 21, 2025. Accessed July 21, 2025. Rajaram R, Spicer JD, Dhupar R, Kim JY, Sepesi B, Hofstetter WL. Esophagus. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 42. Wilder FG, Yang SC. Management of esophageal cancer. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:54-65. | |
| |
Review Date: 1/28/2025 Reviewed By: John Meilahn, MD, General Surgeon, Wyndmoor, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 07/21/2025. The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited. | |

 Esophageal cancer
Esophageal cancer
